Research Article - Der Pharma Chemica ( 2018) Volume 10, Issue 5
Sodium-glucose co-transporter 2 (SGLT2) Inhibitors: New Target for Type 2 Diabetes Mellitus (T2DM) Review
Swapna Vadlamani*
Asst. proffesor, NIPER, Hyderabad, Andhra Pradesh, India
Abstract
Introduction: Knocking out type2 diabetes by new insulin independent renal glucose transporters as targets, reducing the side effects related to high rise in glucose levels is a more efficient way to manage diabetes. Sodium-glucose co-transporter 2 (SGLT2) inhibitors block reabsorption of glucose back into the blood and stimulate secretion in urine in a way controlling blood glucose levels.
Areas discussed: We emphasize in this review an overview of type 2 diabetes. New insulin independent targets, SGLT family inhibitors and their mechanism of action are briefly discussed. Molecular modeling studies carried out for new analogues of SGLT2 were indicated and also about current marketed SGLT drugs their safety issues are briefly outlined.
Conclusion: SGLT2 inhibitors are very promising drugs for near future, where insulin sensitization is a problem. A combination of drugs related to insulin dependent pathway and also independent pathway like SGLT2/SGLT1 drugs will be more effective in glycemic control with lesser side effects.
Keywords
Type II Diabetes, SGLT2 inhibitors
Introduction
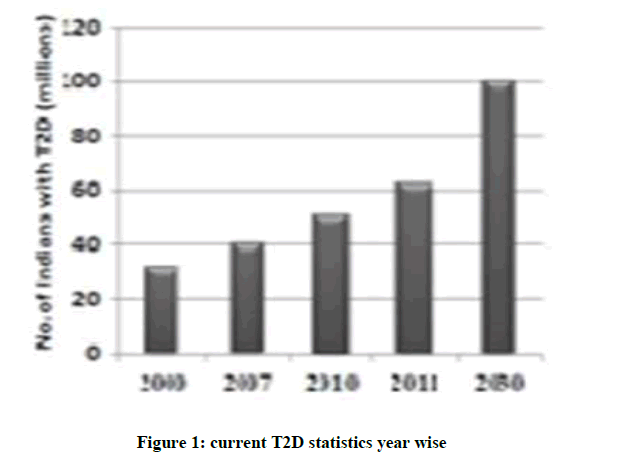
Present scenario of food habits and absolutely very less physical activity is becoming the major cause for obesity finally leading to diabetes. Diabetes is said to be a rich man disease and mostly occurs at the later age of 40, but now one in every 5 persons at early age diagnosed turned to be diabetic mainly because of lifestyle changes. If this situation prevails there is a shoot up of 366 million diabetic patients by 2030 (Figure 1)[1]. Excess weight, physical and family history is the major causes of Type 2 Diabetes Mellitus (T2DM). Environmental and life style factors demands for excess insulin production, finally leading to insulin resistance due to overburden of β cells for insulin production [2,3]. These effects finally turn on impaired metabolism. Current drugs in the market such as Biguanide, Meglitinides, Sulphonylureas and Dipeptidyl peptidase-4 (DPP4) inhibitors,etc. Which are unable to control the glycemic levels for long duration and some are causing weight gain and some causing heart failures (Table 1) [4-6]. There is urgent need for treating T2DM in an alternative manner. New targets SGLT inhibitors were currently studied as they treat T2DM in new approach independent of insulin pathway. These agents provide an insulin-independent means to reduce the hyperglycemia that is the hallmark of the disease by inhibition of a renal transporter thereby blocking the recovery of glucose from the glomerular filtrate [1,4,7]. As a consequence of Sodium Glucose co-Transporter 2 (SGLT2) inhibitions, 50-90 g/day of glucose is eliminated in urine depending on the glycemic level of the individual (Table 2).
| Medication | Average A1C lowering | Hypoglycemic Agent | Weight Gain/Loss |
|---|---|---|---|
| Metformin | 1.50% | No | Loss |
| Sulfonylureas | 1.50% | Yes | Gain |
| Glinides | 1-1.5% | No | Gain |
| SGLT-2 Inhibitors | 1% | No | Loss |
| TZDs | 0.5-1.4% | No | Gain |
| α-Glucosidase Inhibitor | 0.5-0.8% | No | Neutral |
| DPP-4 Inhibitors | 0.5-1% | No | Neutral |
Table 1: The effects of Current diabetic drugs in the market
| S. No. | FDA approved drugs | Company |
|---|---|---|
| 1 | Dabagliflozin | AstraZeneca |
| 2 | Canagliflozin | Mitsubishi Tanabe Pharma and Johnson & Johnson |
| 3 | Emaphagliflozin | Eli Lilly |
| 4 | Remogliflozin Etabonate | GlaxoSmithKline |
| 5 | Sergliflozin Etabonate | GlaxoSmithKline |
| 6 | Tofoglitazone | Roche & Chugal |
| 7 | LX4211 | Lexicon |
| 8 | Ertugliflozin | Pfizer |
| 9 | Ipragliflozin | Astella |
Table 2: Current diabetic drugs
SCL5 family
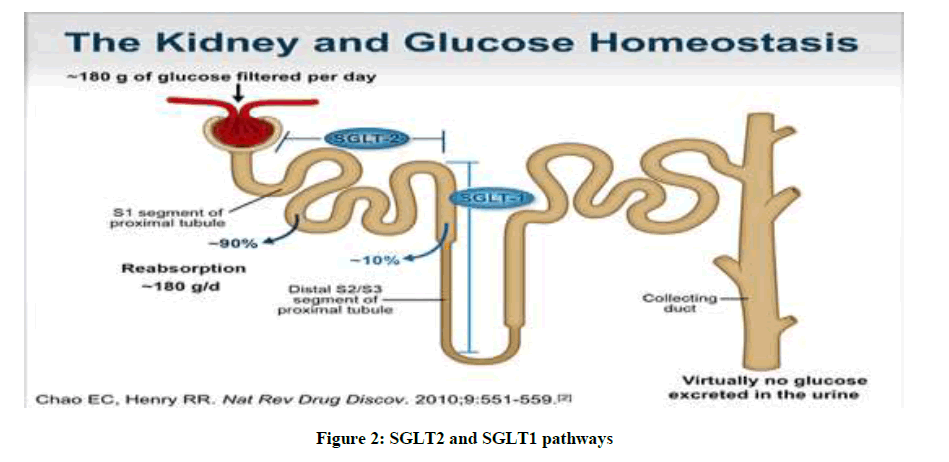
The transport of glucose takes place by different mechanisms. Sodium dependent and sodium independent transporters are involved. The sodium independent transporters belong to SCL2A gene family. Complete structure and functional annotation is only done for two SGLT1 and SGLT2 transporters (Figure 2). SGLT3- SGL2T6 functional annotations is not completely done. Per day around 180 g approximately of D-glucose is filtered back into plasma by these transporters. Most of the sugar is reabsorbed in convoluted proximal tube by a low affinity high capacity (SGLT2) transporter and remaining by SGLT1 a high affinity and low capacity transporter in straight proximal tube. These transporter proteins are of molecular weight 73 KDa and pI of 5.3. These proteins are made up of 14 trans membrane helices with both hydrophobic amino terminal and carboxyl terminal facing extracellular solution. Sodium Glucose Co-Transporter 2 (SGLT2) inhibitor-mediated elimination of glucose represents a fundamentally new paradigm shifting means to treat type 2 Diabetes Mellitus (T2DM) [8]. The major differences between these two transporters are briefly mentioned in the Table 3 below.
| SGLT1 | SGLT2 |
|---|---|
| High affinity | Low affinity |
| Low capacity | High capacity |
| Transports D-glucose/D-galactase and synthetic sugars α-MDG and 3-o-methyl D-glucose | Transports D-glucose/D-galactase and synthetic sugars 3-o-methyl D-glucose |
| Sodium/glucose coupling ratio is 1 | Sodium/glucose coupling ratio is 2 |
| Accession number NP00334 | Accession number NP0030332 |
| Inhibition Ki by Phlozirn in µm is 0.22 | Inhibition Ki by Phlozirn in µm is 1 |
| It is hypothesized that sodium and glucose have separate pathways through SGLT1 Binding of sodium to n-terminal triggers glucose binding | Not clearly known |
| Mutation of this gene resulted in neonatal condition of glucose galactase and malabsorption and also likely to cause gastro intestinal side effects (Gallo, Wright, & Vallon, 2015; Ghezzi et al., 2014) | No serious side effects are reported |
Table 3: Major difference between SGLT2/SGLT2 [10-12]
Scenario of SGLT1/SGLT2 molecules
First natural product which is STGLT1 inhibitor was Phlorizin which is hydrolyzable antagonist. Several non-hydrolyzable antagonists, including O-glycosides (e.g., Sergliflozin, Remogliflozin ) are Susceptible to glucosidase degradation, this was overcome by the discovery of C-glycosides such as Dabagliflozin and Canagliflozin, with increased lipophilicity and molecular weight Additionally, several C-glycosides induce chromosome breaks and/or gain or loss of function in vitro (micronucleus test), with the caveat that in vitro data may not be replicated in vivo. These non-hydrolyzable antagonists are being, or have been, tested to counteract Type II diabetes in mice and humans. Thus, until recently, the primary structures of SGLT2 antagonists have been dominated by the O-glycosides and C-glycosides. Stability wise C-glycosides are more likely druggable candidates than O-glycosides.
Because SGLT2 has been identified as a promising target to treat diabetes, several classes of SGLT2 receptor antagonists were synthesized and investigated including O-glycoside, C-glycoside, and N-glycoside [9,10] Phlorizin, the first SGLTs anti-diabetic agent, isolated in 1835 from the root bark of the apple tree was subsequently found to be a potent but relatively nonselective inhibitor of both SGLT2 and SGLT1, which leads to glucose malabsorption, dehydration, and diarrhea. Even so, it fuelled the search for a Phlorizin derivative that has a higher selectivity of SGLT2 against SGLT1 and fewer sides.
A number of more drug-like O-glucoside-containing analogs have been reported; some, such as T-1095A 2, Sergliflozin A3 and Remogliflozin 4 progressed into early clinical trials [11,12]. However, due to inferior in vivo potency and pharmacokinetic (PK) profile, these were superseded by the C-glucoside dapagliflozin 5 (1.1 nM SGLT2 EC50; 1200-fold selectivity vs SGLT1) and subsequent diarylmethane-containing analogs. Same pharmacophore was employed; rather the Diarylmethane structure in the Bristol-Myers Squibb disclosures was further reworked to establish new proprietary positions. These efforts generally utilized one of two strategies: modification of the glycone component or alteration of a structural element of the glucose moiety Ertugliflozin, incorporating a structurally novel dioxa-bicyclo-[3.2.1] octane ring system, and de rivatives form a third class of potent and selective SGLT2 antagonists [13-15].
Molecular docking of empagliflozin analogues (Table 4)
Docking studies have been conducted for the 13 analogues of Empagliflozin. The molecular modeling studies are done by Schrodinger software. The accession number for SGLT2 (NP0030332) is given in PDB site and corresponding protein sequences are retrieved. The protein structure using MODLER is modeled and further docking studies have been carried out. Based on the docking score and the active pharmacophore interactions best suitable molecules of high potential activity are listed.
| S. No. | Structure | Glide score | Interactions |
|---|---|---|---|
| 1 | 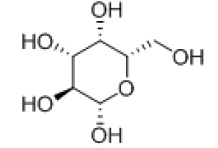 |
-7.389 | H-bond: GLU-68, GLN-428, TRP-264, GLU-88, Hydrophobic:ALA-259, LUE-256, TYR-263, MET-73, VAL-301, Pi-pi-stackings: TYR-263 |
| 2 | 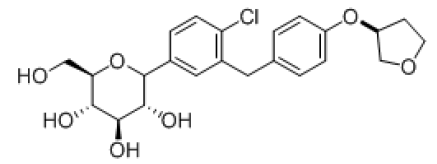 |
-7.2269 | H-bond- GLU-68, GLU-88, Hydrophobic-: ALA-259, LUE-256, TYR-263, MET-73, VAL-301, TYR-138, Pi-pi-stackings: TYR-263 |
| 3 | 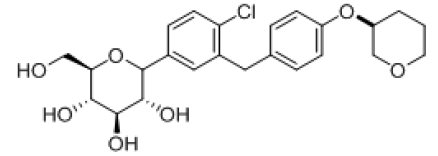 |
-7.763 | H-bond- GLU-68, GLU-88, ALA-63, GLN-428, Hydrophobic- ALA-259, LUE-256, TYR-263, MET-73, VAL-301, TYR-138, Pi-pi-stackings: TYR-263 |
| 4 | 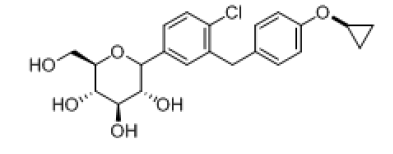 |
-7.064 | H-bond- GLU-68, GLU-88, ALA-63, GLN-428, Tyr-263, Hydrophobic-LUE-137, TYR-262, ALA-259, MET-369, Pi-pi-stackings: TYR-263 |
| 5 | 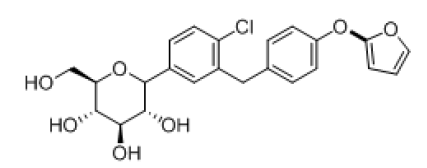 |
-8.064 | H-bond- GLU-68, GLU-88, LYS-294, GLN-69, GLN-428, Hydrophobic-LEU-137, MET-73,VAL-258, ALA-63, TRP-263, TYR-138, Pi-pi-stackings: TYR-263 |
| 6 | 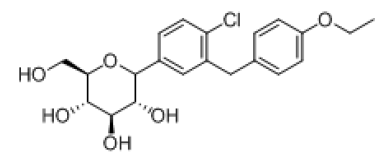 |
-8.103 | H-bond- GLU-68, GLU-88, TYR-138, ASN-267, ALA-63, Hydrophobic- LEU-137, MET-73, VAL-141, ALA-63, TRP-134, TYR-138, Pi-pi-stackings: TYR-263 |
| 7 | 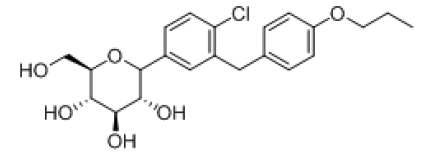 |
-8.24 | H-bond-- GLU-68, GLU-88, TYR-263, ASN-267, ALA-63, GLN-69, Hydrophobic- LEU-137, MET-73, VAL-258, ALA-63,TRP-263, TYR-262, Pi-pi-stackings: TYR-263 |
| 8 | 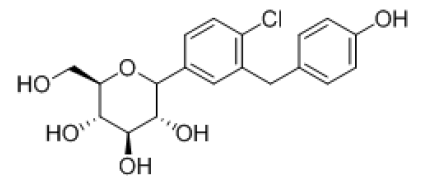 |
-8.59 | H-bond- GLU-68, GLU-88, ASN-267, GLN-69, GLN-428, SER-91, LYS-294, Hydrophobic- LEU-256, MET-73, VAL-258, TRP-263, TYR-138, Pi-pi-stackings: TYR-263 |
| 9 | 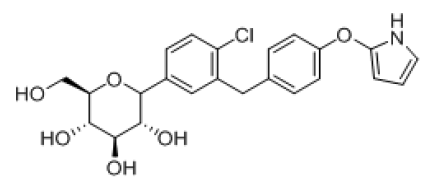 |
-6.98 | H-bond- GLU-68, GLU-88, ALA-63, TRP-264, LUE-137, TYR-263, Hydrophobic- LEU-137, MET-73, VAL-258, ALA-63, TRP-263, TYR-138, Pi-pi-stackings: TYR-263 |
| 10 | 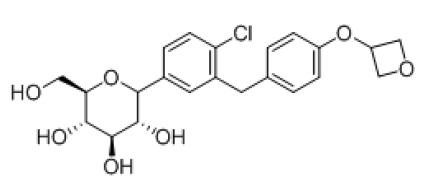 |
-7.448 | H-bond-- GLU-68, GLU-88, LYS-294, TRP-264, ASN-64, TYR-263, ALA-63, Hydrophobic- LEU-137, MET-73,VAL-258, ALA-63, TRP-263, TYR-138, Pi-pi-stackings: TYR-263 |
| 11 | 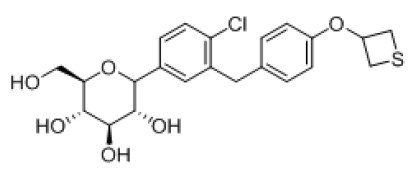 |
-7.218 | H-bond--- GLU-68, GLU-88, LYS-294, TRP-264, ASN-64, TYR-263, ALA-63, Hydrophobic- LEU-137, MET-73, VAL-258, ALA-259, TRP-263, TRP-262, Pi-pi-stackings: TYR-263 |
| 12 | 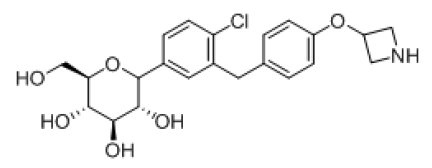 |
-6.796 | H-bond-GLU-68, GLU-88, LYS-294, GLN-69, GLN-428, SER-91, Hydrophobic- LEU-137, MET-73, VAL-258, ALA-259, TRP-263, TRP-262, Pi-pi-stackings: TYR-263 |
Table 4: Molecular Docking of Empagliflozin Analogues
Conclusion
SGLT2 inhibitors are currently promising molecules for treating Type 2 diabetes. Combined therapy based on Insulin dependent drugs altogether with insulin independent drugs will be a better strategy to have good control over diabetes. In this review molecular modeling studies were carried out and the outcome molecules were having very good Glide score and they could be future promising molecules for controlling T2DM.
References
- L. Guariguata, D.R. Whiting, I. Hambleton, J. Beagley, U. Linnenkamp, et al., Diabetes. Res. Clin. Pract., 2014, 103(2), 137-149.
- E.H. El Ashry, L.F. Awad, H.A. Hamid, A.I. Atta, J. Carbohydr. Chem., 2007, 26(5-6), 329-338.
- M.Kern, N. Klöting, M. Mark, E. Mayoux, T. Klein, et al., Metabolism., 2016, 65(2), 114-123.
- M. Hrapchak, B. Latli, X. Wang, H. Lee, S. Campbell, et al., J. Labelled. Comp. Radiopharm., 2014, 57(12), 687-694.
- L. Rossetti, D. Smith, G.I. Shulman, D. Papachristou, R.A DeFronzo, J Clin Invest., 1987, 79(5), 1510-1515.
- W. Meng, A.B. Ellsworth, A.A. Nirschl, P.J. McCann, M. Patel, et al., J. Med. Chem., 2008, 51(5), 1145-1149.
- J.R.L. Ehrenkranz, N.G. Lewis, C.R. Kahn, J. Roth, Diabetes. Metab. Res. Rev., 2005, 21(1), 31-38.
- X.J. Wang, L. Zhang, D. Byrne, L. Nummy, D. Weber, et al., Org. Lett., 2014, 16(16), 4090-4093.
- W.N. Washburn, Expert. Opin. Ther. Pat., 2012, 22(5), 483-494.
- C. Wanner, S.E. Inzucchi, J.M. Lachin, D. Fitchett, M.V. Eynatten, et al., N. Engl. J. Med., 2016, 375(4), 323-334.
- S. Lemaire, I.N. Houpis, T. Xiao, J. Li, E. Digard, et al., Org. Lett.,2012, 14(6), 1480-1483.
- N.C. Goodwin, R.M., B.A. Harrison, M.K. Shadoan, Z.Y. Almstead, et al., J. Med. Chem., 2009, 52(20), 6201-6204.
- S. Kasichayanula, X. Liu, M.P. Benito, M. Yao, M. Pfister, et al., Br. J. Clin. Pharmacol., 2013, 76(3), 432-444.
- B. Kumari, D. Chetia, Int. J. Pharm. Pharm. Sci., 2013, 5(2), 633-638.
- S. Kohler, A. Salsali, S. Hantel, S. Kaspers, H.J. Woerle, et al., Clin. Ther., 2016, 38(6), 1299-1313.