Research Article - Der Pharma Chemica ( 2023) Volume 15, Issue 6
Review on: Floating Drug Delivery System
Aishwarya V Deshmukh*, SR Gawande and AV ChandewarAishwarya V Deshmukh, Department of Pharmaceutical Sciences, Pataldhamal Wadhwani College of Pharmacy, Yavatmal, India, Email: aishwaryadeshmukhkalamb@gmail.com
Received: 28-Oct-2023, Manuscript No. Dpc-23-119633; Editor assigned: 31-Oct-2023, Pre QC No. Dpc-23-119633 (PQ); Reviewed: 14-Nov-2023, QC No. Dpc-23-119633; Revised: 17-Nov-2023, Manuscript No. Dpc-23-119633 (R); Published: 15-Dec-2023, DOI: 10.4172/0975-413X.15.6.142-146
Abstract
Floating matrix tablets were developed to prolong gastric residence time and increase drug absorption further increasing the bioavailability. Various forms of gastro retentive drug delivery system, such as floating and non-floating. Floating tablets was formulated to increase gastric residence and there by improve its therapeutic efficacy. By using different polymers such as carbopol, guargum, HPMC K100, HPMCK4 etc. Formulated tablets showed satisfactory results for various post compression evaluation parameters like thickness, hardness, weight variation, floating lag time, total floating time, content uniformity and in vitro drug release.
Keywords
Floating Drug Delivery System; Floating tablets; GRDDS; Drug release
Introduction
In 1968, Davis first inventor of floating drug delivery system. The oral route is considered as the most favorable route of drug delivery. Gastric emptying of dosage forms is an extremely variable process and ability to prolong and control emptying time is a valuable asset for dosage forms, which reside in the stomach for a longer period of time than conventional dosage forms. Unpredictable Gastric Residence Time (GRT) of a controlled release dosage form leads to interest in targeting and retaining the dosage form in the stomach for a prolonged period of time. Thus Retention of drug delivery systems in the stomach prolongs overall gastrointestinal transit time and improves the oral bioavailability of the drugs that are having site-specific absorption from the stomach or upper part of the small intestine. The high level of patient compliance has been observed in taking oral dosage forms is due to the ease of administration and handling of these forms. There are lot of advancements have been seen in oral controlled drug delivery system in the last few decades, this system has been of limited success in case of drugs with a poor absorption window throughout the GIT (Gastro Intestinal Tract). To modify the GIT time is one of the main challenge in the development of oral controlled drug delivery system [1-3].
Materials and Methods
Stomach
The main function of stomach is to store food temporarily grind it and then release it gradually into the duodenum. The stomach is the important site of enzyme production. Compare to small intestine the absorption from stomach is low due to its small surface which acts as a barrier for the delivery of drug to small intestine. Gastro intestinal motility is based on fasted and fed state of the stomach, two distinct patterns of Gastrointestinal (GI) motility and secretions have been identified [4-7].
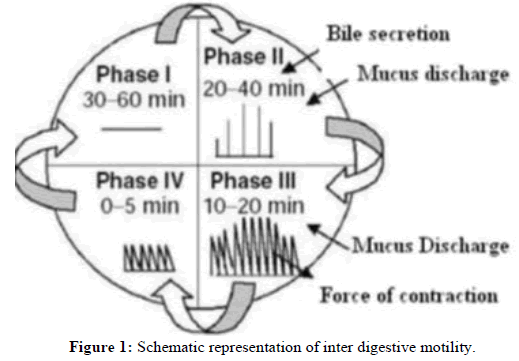
Phase I: It is an inactivity period lasting from 30 to 60 min with no contractions and is characterized by absence of secretory, electrical and contractile activity. It is also called basal phase.
Phase II: It is also called as pre-burst phase it consists of intermediate active contractions that gradually increase in intensity and frequency as the phase progresses and it lasts about 20 to 40 min.
Phase III: This is a short period of intense distal and proximal gastric contractions this is 4-5 contractions per min due to this contraction all the undigested material is cleared out of the stomach down the small intestine .It is also known as “house keeper waves”.
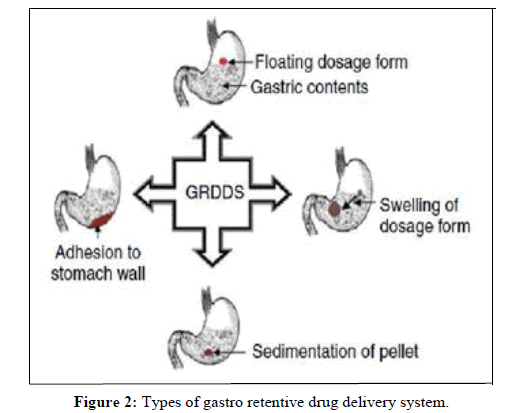
Phase IV: This is the short period of about 0 to 5 min and contractions disparate between the last part of the phase III and quiescence of phase I (Figures 1 and 2).
Results and Discussion
Classification of floating type drug delivery system
Floating systems: Floating Drug Delivery Systems (FDDS) have a bulk density lower than gastric fluids and thus remain buoyant in the stomach for a prolonged period of time, without affecting the gastric emptying rate. While the system is floating on the gastric contents, the drug is released slowly at a desired rate from the system. After the release of the drug, the residual system is emptied from the stomach. This results in an increase in the GRT and a better control of fluctuations in the plasma drug concentrations.
Floating systems can be classified into two distinct categories, effervescent and non-effervescent systems.
Single unit floating dosage system:
• Effervescent system (gas generating system).
• Non-effervescent systems.
• multiple unit floating dosage systems.
Non-effervescent systems:
• Effervescent system (Gas generating system).
• Hollow microsphere.
• Raft forming system.
Mechanism of FDDS
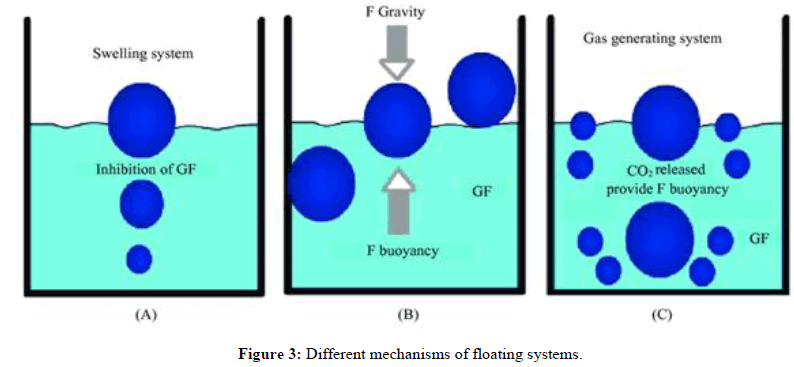
There are various attempts have been made to retain the dosage form in the stomach as a way of increasing the retention time. These attempts include introducing the floating dosage form as gas generating system and swelling system modified shape system. Gastric emptying delaying devices and co-administration of gastric emptying delaying drugs. Among these, the floating dosage form has been most commonly used. Floating drug delivery systems have a bulk density less than gastric fluid and so remain buoyant in the stomach without affecting the gastric emptying rate for a prolong period of time. While the system is floating on the gastric content (Figure 3) [8-10].
F =F buoyancy-F gravity=(Df-Ds)gv
Where,
F=Total vertical force
Df=Fluid density
Ds=Object density
V=Volume
G=Acceleration due to gravity
Factors affecting FDDS
Density: Floating is a function of dosage form buoyancy that is dependent on the density.
Shape of the dosage form: Ring shaped and tetrahedron device with flexural modules of 48 and 22.5 Kilo pounds per Squares Inch (KSI) are reported to have better floating, 90% to100% retention at 24 hours as compared with other shapes.
Concomitant drug administration: Anticholinergic like atropine and propantheline, prokinetic agents like metoclopramide and cisapridecan affect floating time
Fed or unfed state: Under fasting conditions the GI mobility is characterized by periods of strong motor activity or the Migrating Myoelectric Complex (MMC) that occurs every 1.5 to 2 hours.
Nature of meal: Feeding of indigestible polymers or fatty acid salts can change the motility pattern of the stomach to a fed state, thus decreasing the gastric emptying rate and prolonging drug release.
Caloric content and feeding frequency: Floating can be increased by four to 10 hours with a meal that is high in protein and fats. The floating can increase by over 400 minutes when successive meals are given compared with a single meal duty low frequency of MMC.
Age: Elderly people, especially those over 70, have a significantly longer; floating, disease condition such as diabetes and crohn`s disease etc. also affect drug delivery.
Posture: Floating can vary between supine and upright ambulatory states of the patents.
Advantages of FDDS
•FDDS reduces the drug concentration fluctuation that makes it possible to obtain certain selectivity in the exact pharmacological effect ofdrugs that are supposed to activate different types of receptors at different concentrations.
•Slow release of the drug into the body reduces the counter activity to minimum level leading to higher drug efficiency.
•Retention of the drug in the gastric formulation at stomach minimizes the amount of drugs that reaches the colon, thereby preventing thedegradation of drug that degrades in the colon.
•GRDDS is highly advantageous in case of drugs having local action e.g., antacids.
•Possible reduction in dosing and improved patient compliance thanks to ease of administration.
•Economic use of dosage forms.
•Drugs that are absorbed through the stomach are advantageous (e.g., antacids).
•Achieves microbiological and chemical stability compared to other oral routes.
•Enhanced activity span for short half-life drugs.
•Enhanced bioavailability and therapeutic efficacy of the drugs.
•Reduction of intra and inter subject variability in plasma drug levels.
•Increased pH solubility of drugs.
•Fewer side effects and optimized therapy.
•Improved selectivity in receptor activation.
•Accommodates site specific drug delivery systems.
Disadvantages of FDDS
• Not practicable for drugs that have stability or solubility problem in the upper gastrointestinal tract.
• Some drugs arranged for the buoyant system may cause irritation and lesions to gastric mucosa.
• Heightened fluid levels are essential inside the stomach for the drug to float sufficiently.
• Difficulty estimating the detailed motility of the stomach.
• Swelling system should be rapid acting once the drug reaches the stomach.
| Types of dosage forms | Drugs explored in floating dosage forms |
|---|---|
| Microspheres | Aspirin, griseofulvin, P-nitro aniline, ibuprofen, ketoprofen, terfenadine, tranilast . |
| Granules | Diclofenac sodium, indomethacin, prednisolone. |
| Films | Cinnarizine, drug delivery device. |
| Capsules | Chlordiazepoxide HCl, diazepam, furocemide , L-dopa and benserazide, misoprostol, nicardipine, propranolol HCl, ursodeoxychoric acid. |
| Tablets/pills | Acetaminophen, aspirin, amoxycillin trihydrate, ampicillin, atenolol, captopril, ciprofolxacin, chlorpheniramine maleate, cinnarizine, furosemide, 5-Fluorouracil, isosorbide mononitrate, diltiazem, Isosorbide dinitrate, nimodipine, para amino benzoic acid, prednisolone, quinidine, varapamil HCl, riboflavin, sotalol. |
Table 1: List of drugs explored in floating dosage form.
Polymers used in floating drug delivery system
Polymers are used in floating system so as to target the drug delivery at specific region in the GI tract i.e., stomach. Both synthetic and natural polymers are used in the floating drug delivery. Natural polymers used in floating system are guar gum, chitosan, xanthan gum, gellan gum, sodium alginate, etc. Synthetic polymers used for the floating drug delivery are HPMC, Eudragit, ethyl cellulose, etc [10-14].
Applications of floating microspheres
• Floating microspheres can be used as carriers for drugs with so called absorption windows, these substances, for example antiviral,
antifungal and antibiotic agents (sulphonamides, quinolones, penicillin’s , cephalosporin’s, amino glycosides and tetracycline’s) are taken
up only from very specific sites of the GI mucosa.
• Hollow microspheres of non-steroidal anti-inflammatory drugs are very effective for controlled release and reduce the major side effect of
gastric irritation. For example, floating microspheres of indomethacin are quite beneficial for rheumatic patients.
• Hollow microspheres can greatly improve the pharmacotherapy of the stomach through local drug release, leading to high drug
concentrations at the gastric mucosa, thus eradicating Helicobacter pylori from the sub mucosal tissue of the stomach and making it
possible to treat stomach and duodenal ulcers, gastritis and esophagitis.
Evaluation of formulations
• Pre compression parameters were including angle of repose, bulk density, tapped density ,car’s index and last Hausners ratio.
• Post compression parameter were including weight variation, hardness, friability, thickness and diameter, in vitro buoyancy studies ,
swelling index and in vitro dissolution studies.
Conclusion
Floating matrix tablets were developed to prolong gastric residence time and increase drug absorption further increasing the bioavailability. Formulated tablets showed satisfactory results for various post compression evaluation parameters like: tablet thickness, hardness, weight variation, floating lag time, total floating time, content uniformity and in vitro drug release. Different polymers have been evaluated in the design of gastric floating drug delivery. In the present investigation different polymers are used for the matrix formation, HPMC is a very good vehicle.
References
- Dongare PS, Darekar AB, Gondkar SB, et al. Int J Pharma Bio Sci. 2013; 3(4): p.72-85.
- Aundhia C, Shah N, Patel S, et al. Int J Curr Pharm Res. 2020; 12(1): p. 34-35.
- Jindal S, Sharma A, Jindal K. Int J Pharm Sci. 2015; 6(3): p. 2146-2150.
- Subbarao K, Suresh G. Am J Pharm Educ. 2018; 8(4): p.34-37.
- Ramakrishna G, Madhavarao B, Rao DS, et al. Int J Pharm Chem Biol Sci. 2015; 5(4): p.77-80.
- Renuka U. Int J Sci Res. 2017; 14(7): p. 23-25.
- Datir SK, Patil PB, Saudagar RB. J drug deliv ther. 2019; 9(2): p. 428-432.
- Kadwal M, Gnanarajan G, Kothiyal P. J Pharm Innov. 2019; 9(2): p. 228-372.
- Prasanna MM, Pashikanti S. Nat Polym. 2007; 8(2): p. 78-87.
- Dhiman S, Singh TG, Rehni AK, et al. Asian J Pharm Clin Res. 2011; 4(1): p. 5-13.
- Başarir NS, Mesut B, Ozsoy Y. Am J Pharm Res. 2021; 4(2): p. 43-64.
- Neetika B, Manish G. Drud Del Syst. IJPRAS. 2012; 1(4): p. 20-28.
- Ganesh K, Archana D, Preeti K. Int J Pharm Life Sci. 2013; 2(4): p. 165-178.
- Mukund JY, Kantilal BR, Sudhakar RN. Braz J Pharm Sci. 2012; 48(7): p. 17-30.