Review Article - Der Pharma Chemica ( 2024) Volume 16, Issue 4
Periodontal Ligament Stem Cells (PDLSC): A Promising Strategy for Periodontal Regeneration
Nilofer Farjana Habeeb Rahman*, Mohan Valiathan and Anitha BalajiNilofer Farjana Habeeb Rahman, Department of Periodontics, Bharath Institute of Higher Education and Research, Chennai, India, Email: farjanajahangeer@gmail.com
Received: 05-Jul-2024, Manuscript No. DPC-24-140938; Editor assigned: 10-Jul-2024, Pre QC No. DPC-24-140938 (PQ); Reviewed: 24-Jul-2024, QC No. DPC-24-140938; Revised: 01-Aug-2024, Manuscript No. DPC-24-140938 (R); Published: 29-Aug-2024, DOI: 10.4172/0975- 413X.16.4.400-405
Abstract
The presage for the treatment of inflammatory periodontal disease is periodontal regeneration. The cellular therapeutic remedy is an emerging promising strategy in regenerative medicine/dentistry, particularly making use of mesenchymal-derived stem cells. MSC has the capacity to develop into adipogenic, osteogenic/odontogenic and neurogenic cells. Dental stem cells isolated from mature/immature teeth are dental pulp stem cells, stem cells from exfoliated deciduous teeth, periodontal ligament stem cells, stem cells from apical papilla and dental follicle progenitor cells. Periodontal Ligament Stem Cells (PDLSCs) are highly predictable in providing a cell source that can regenerate the lost periodontal structures. In this review, we explore the potential of PDLSCs for periodontal regeneration.
Keywords
Periodontal disease; Periodontal regeneration; Cellular therapy; Stem cells; Periodontal Ligament Stem Cells (PDLSCs)
Introduction
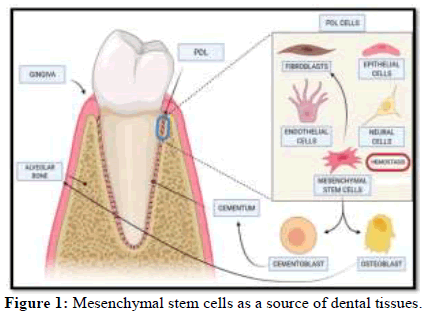
Teeth represent a fascinating area of study in regenerative medicine, because of their unique and complex developmental origin. Stem cells are undifferentiated cells that are capable of self-renewal or differentiation into a specialized cell. They exist within areas of the body known as biological niches and are essential for growth during childhood and homeostasis throughout adulthood. Stem cells can be derived from umbilical cord, amniotic liquid, adipose tissue and bone marrow. Based on the differentiating potential stem cells can be divided into totipotent, pluripotent and multipotent stem cells. Based on the origin stem cells can be divided into embryonic stem cells, adult stem cells and induced pluripotent stem cells. Dental Stem Cells (DSCs), an important source of Mesenchymal Stem Cells (MSCs) as shown in Figure 1, can be easily obtained by minimally invasive procedures and have been used for the treatment of various diseases. MSCs differentiate into angiogenic, neurogenic and osteo/odontogenic cells [1]. Also it has immunomodulatory and paracrine effects [2-4]. Numerous studies have provided evidence of DPSCs' differentiation capacity, such as in neurogenesis, adipogenesis, osteogenesis, chondrogenesis, angiogenesis and dentinogenesis.
DPSCs are considered to be good sources for the regeneration of dental tissue for four primary reasons:
• They are easy to access during surgery and easy to keep alive after
• They generate more dentin tissue faster than stem cells that don't come from the teeth
• They can be cryopreserved and combined in various tissue regeneration support structures
• They have anti-inflammatory properties which are helpful in all transplantation (transplanting tissue from the same species)
Literature Review
There are five types of dental stem cells. They are as follows:
Exfoliated deciduous teeth (SHED), Periodontal Ligament Human Stem Cells (PDLSC), Stem Cells from Apical Papilla (SCAP) and Dental Follicle Progenitor Cells (DFPC) [5-12]. Our point of interest is on the periodontal ligament stem cells. PDLSC can be isolated from cryopreserved periodontal ligaments. PDLSC are multipotent cells that can differentiate into osteogenic, adipogenic, neurogenic and chondrogenic cells in vitro. Most importantly, PDLSC are capable of differentiation into cells similar to periodontium. After transplantation of ex vivo expanded PDLSC into immunocompromised mice, cementum/PDL-like structures were formed, suggesting PDLSC as new therapeutic agents in reconstructive dentistry. PDLSC can be successfully re-implanted into periodontal defects where they promote periodontal regeneration.
Periodontal ligament stem cells
PDLSC, similar to DPSC, have immuno-suppressive characteristics. These cells are able to produce Indoleamine 2, 3-Dioxygenase (IDO), TGFbeta 1 and Hepatocyte Growth Factor (HGF). However, it is interesting to note that secretion of all these factors is mediated by IFN gamma produced by activated peripheral blood mononuclear cell during inflammation. PDLSCs also express other surface markers similar to BMMSCs, such as CD9, CD10, CD13, CD29, CD44, CD49d, CD90, CD105, CD146 and CD166 [13].
The absence of expression of costimulatory factors such as major histocompatibility complex class II antigen, CD40 and CD80, have been highlighted as responsible for the low immunogenicity of MSCs. Further evidence demonstrated the mechanisms activated by mesenchymal cells from periodontal tissues that could result in modulation of the host response. Therefore, in addition to their low immunogenicity/compatibility, MSCs perform their function by suppressing the function of a range of immune response cells and by improving immune regulatory functions. As a result of these activities, MSCs became a prominent alternative for the immune therapy of chronic inflammatory disorders, such as periodontitis. Alongside the natural potential of PDLSCs to be used in regulating the host response in periodontitis, more recently MSCs of dental origin have also been mentioned as possible sources for cell therapy in other cases of inflammatory imbalance-related disorders, such as those affecting the brain (e.g., Alzheimer's disease, Parkinson's disease) and gut (e.g., Crohn’s disease, colitis). Recently, PDLSCs were used to control colitis in an in vivo model and the authors concluded that their immunomodulatory activity was mediated by a group of deoxyribonucleic acid demethylases of the teneleven translocation family.
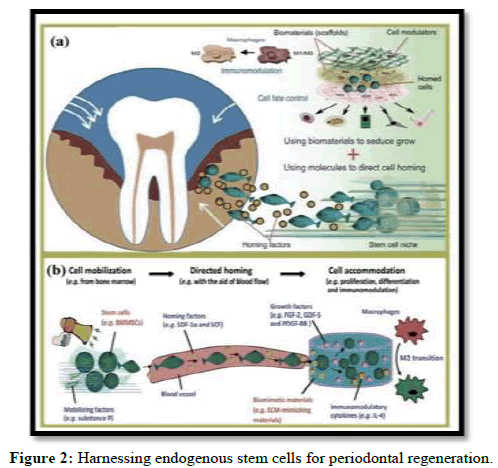
Periodontal regeneration
Tissue engineering is a promising treatment strategy for periodontal disease. It regenerates the completely lost periodontal structures namely gingiva, cementum, periodontal ligament and alveolar bone. Tissue engineering was proposed as a field that would apply the principles of human biology and engineering to the development of functional substitutes for damaged tissues. This strategy should be based on three strategies: (1) cells; (2) scaffolds; and (3) signaling molecules. Regeneration of periodontal tissues takes place by combining PDLSCs in scaffolds and signaling molecules. PDLSCs exhibit a multipotent differentiation capacity and are good candidates for use in tissue engineering due to their potential to promote the regeneration of dental and nondental tissue. They have a better regenerative capacity and maximum potential for signaling molecules and scaffolds for periodontal regeneration as shown in Figure 2 [14].
Discussion
Tissue engineering using PDLSCs can also assist in the neoformation of periodontal tissues on the titanium surface of dental implants, facilitating their fixation and providing better mechanical and immunological properties in patients with a previous history of tooth loss treated by implant replacement therapy. Studies have reported that the use of PDLSCs sheets on the surface of titanium implants stimulate the formation of cementumlike and periodontal ligament like tissues, both in xenogenic and autologous models (Tables 1 and 2) [15-20].
|
Bone regeneration | PL | Cementum |
|---|---|---|---|
| BMMSC | Effective in grade III furcation defects, but bone fill is not complete; Ineffective when used without bone substitutes | Effective in grade III furcation defects; conflicting results; effective only associated with bone substitutes. | Effective in grade III furcation defects. |
| ASC | Effective in extraction sockets. |
Effective in surgically created intrabony defects. | Effective in surgically created intrabony defects. |
| PDLSC | Effective in fenestration; no added benefit associated with non reservable membranes in fenestrations; effective in intrabony defects only using bone substitutes. |
Effective in fenestration; more effective than BMMSC; effective in intrabony defects with better results using bone substitutes. | Effective in fenestration; added benefit associated with non reservable membranes in fenestrations: effective in intrabony defects with better results using bone substitutes. |
| DPSC | Effective in extraction sockets; improve bone regeneration in intrabony defects. |
Improve regeneration in intrabony defects. | Improve regeneration in intrabony defects. |
| DFPC | Improve effects of PDLSC. | Improve effects of PDLSC. | Improve effects of PDLSC. |
| SHED | Increased bone volume in intrabony defects | Increased PL fibres in intrabony defects. | Increased in intrabony defects. |
| SCAP | Increased bone volume in intrabony defects compared to saline. | Increased in intrabony defects compared to saline. | Increased in intrabony defects compared to saline. |
Note: BMMSC: Bone Marrow Mesenchymal Stem Cell; ASC: Adipose Derived Stem Cell; PDLSC: Periodontal Ligament Stem Cell; DPSC: Dental Pulp Stem Cell; DFPC: Dental Follicle Precursor Cell; SHED: Stem Cell from Human Exfoliated Teeth; SCAP: Stem Cell from Apical Papilla
Table 1: Periodontal regeneration with mesenchymal stem cells.
| Cell type | Animal model | Analysis | Results |
|---|---|---|---|
| BMSC | DOG Beagle female 12-20 months old |
|
BMSC group showed neocementum along the denuded dentin with bone ligament formation. No root resorption or ankylosis reported. |
| BMSC | DOG Beagle female 12-20 months old |
|
Defects treated with MSC showed newly formed of cementum, PL and alveolar bone. |
| BMSC | DOG Mongrel |
|
All the groups with PRP showed regeneration of bone and cementum. BMSC showed the best potential for periodontal regeneration. |
| BMSC | DOG Mongrel male 14-22 kg |
|
Test group showed higher percentage of cementum and PL regeneration. Bone formation was equal in test and control group. |
| rADSCs rDPSCs |
New Zealand withe RABBIT 2-12 months old |
|
Genetic expression of ASCs and DPSCs are similar. Transplanted ASCs regenerate PL, and alveolar bone. |
| PDLSC | MINIATURE PIG female Wuzhishan, male Guizhou 6-8 months old |
|
Bone, cementum and ligament resulted regenerated in both allogenic and autogenous PDLSC. |
| PDLSC SHED |
MINIATURE PIG Female 9-12 months old |
|
Both cell types improved regeneration |
| PLSC DPSC |
MINIATURE PIG 18 months old |
|
PL and bone tissue had been generated in both groups. |
| PDLSC | DOG Beagle |
|
No differences were found between autologous and allogenic groups. a) and c) showed collagen fibers oblique and parallel to the root. b) had perpendicularly inserted fibers in new cementum. |
| PDLSC BMSC |
MINIATURE PIG 2 years old |
|
PL regeneration was found in both groups. |
| CDC PDLSC |
DOG Beagle male 1 year old |
|
Test group showed higher percentages of new cementum, associated with higher attachment gains. No increased bone regeneration was found. |
| PDLC | DOG Beagle female 3 years-old |
|
Group with PDLC showed more cementum, bone and ligament formation. |
| PDLSC | DOG Beagle female |
|
No differences in bone formation between the groups, but PDLSC showed more cementum formation. |
| PDLC | DOG Beagle male |
|
Control group showed limited new bone formation while the addition of PDLC resulted in bone and cementum regeneration. |
| PDLSC | MINIATURE PIG 12 months old |
|
PDLSC showed bone, ligament and cementum regeneration. Good orientation of the anchoring fibers was found. |
| PDLC | DOG 18-36 months old |
|
Cementum, bone heights and surface were more significant in group a. |
| DPSC | DOG Mongrel male1-2 years old |
|
Bone formation was similar between the groups. Cementum and ligament were regenerated more in the test group. |
| PDLSC SHED |
MINIATURE PIG female 9-12 months old |
|
PDLSC and SHED significantly improved periodontal regeneration. |
| GMSC | MINIATURE PIG 1 female and 7 males 18 ± 1 months old |
|
Better results were found for groups with GMSC. |
| ASC | DOG Beagle female 50-56 months old |
|
New alveolar bone, PL and cementum were found at sites treated with ASC. |
| ASC | DOG Beagle 9 or 10 months old |
|
Periodontal regeneration only occurred in test group. |
Note: HA: hydroxyapatite; TCP: Tricalcium Phosphate; PGA: Polyglycolic Acid; ePTFE: e-Polytetrafluoroethylene; PRP: Platelet-Rich Plasma; DPSC: Dental Pulp Stem Cells; PDLSC: Periodontal Ligament Stem Cells; PDLC: Periodontal Ligament Cells; DFSC: Dental Follicle Stem Cells; CDC: Cementum Derived Cells; GMSC: Gingival Margin Stem Cells; SHED: Stem Cells From Human Exfoliated Deciduous Teeth; BMSC: Bone Marrow Stem Cells; ASC: Adipose Stem Cells; MSC: Mesenchymal Stem Cells; AC: Atelocollagen; PL: Periodontal Ligament; CAL: Clinical Attachment Level; PI: Plaque Index; PD: Probing Depth; GR: Gingival Recession; BOP: Bleeding On Probing; HES: Hematoxylin Eosin Stain; Col: Collagen; GFP: Green Fluorescent Protein; CRP: Serum C-Reactive Protein; IL-10: Interleukin-10; CD: Cluster Of Differentiation; SEM: Scanning Electron Microscopy
Table 2: Periodontal regeneration with mesenchymal stem cells in animal studies.
Conclusion
The discovery of Periodontal Ligament Stem Cells (PDLSCs) highlighted the possibility for development of tissue engineering technology based therapeutics for disrupted periodontium. PDLSCs are a kind of somatic stem cells that show potential to differentiate into multiple cell types and undergo robust clonal self-renewal. Therefore, PDLSCs are considered a highly promising stem cell population for regenerative therapy in periodontium; however, their rarity prevents the progression of basic and clinical researches. In this review, we summarize recent research advancement and accumulated information regarding the self-renewal capacity, multipotency and immunomodulatory effect of PDLSCs, as well as their contribution to repair and regeneration of periodontium and other tissues. We also discuss the possibility of PDLSCs for clinical application of regenerative medicine and provide an outline of the genetic approaches to overcome the issue about the rarity of PDLSCs.
In summary, the regenerative and therapeutic potential of PDLSCs seems to be auspicious from a biological perspective. No clinical evidence of their application with specific use for immunomodulatory periodontology/medicine has been reported so far. Despite some promising clinical results and biological insights herein discussed. Several gaps need to be filled before adopting a protocol for their clinical use in patients with periodontitis or other inflammatory conditions.
In this sense, we draw attention to the fact that most studies associate PDLSCs with osteoinductive/osteoconductive materials. These materials, especially those synthetic and xenogenic, can affect therapeutic efficacy and safety by reducing mechanical properties, impairing bone remodeling and inducing an immunological reaction.
References
- Horwitz EM, Le Blanc K, Dominici M, et al. Cytotherapy. 2005; 7(5): p. 393-395.
[Crossref] [Google Scholar] [PubMed]
- Gnecchi M, Danieli P, Malpasso G, et al. Mesench Stem Cells: Met Prot. 2016: p. 123-46.
[Crossref] [Google Scholar] [PubMed]
- Kot M, Musiał-Wysocka A, Lasota M, et al. Acta Biochim Pol. 2019; 66(4): p. 499-507.
[Crossref] [Google Scholar] [PubMed]
- Wada N, Gronthos S, Bartold PM. Periodontology. 2013;63(1): p. 198-216.
[Crossref] [Google Scholar] [PubMed]
- Gronthos S, Mankani M, Brahim J, et al. Proc Natl Acad Sci USA. 2000; 97(25): p. 13625-13630.
[Crossref] [Google Scholar] [PubMed]
- Miura M, Gronthos S, Zhao M, et al. Proc Natl Acad Sci. 2003; 100(10): p. 5807-5812.
[Crossref] [Google Scholar] [PubMed]
- Seo BM, Miura M, Gronthos S, et al. Lancet. 2004; 364(9429): p. 149-155.
[Crossref] [Google Scholar] [PubMed]
- Sonoyama W, Liu Y, Fang D, et al. PloS one. 2006; 1(1): p. 79.
[Crossref] [Google Scholar] [PubMed]
- Morsczeck C, Götz W, Schierholz J, et al. Matrix Biol. 2005; 24(2): p. 155-165.
[Crossref] [Google Scholar] [PubMed]
- Matsubara T, Suardita K, Ishii M, et al. J Bone Miner Res. 2005; 20(3): p. 399-409.
[Crossref] [Google Scholar] [PubMed]
- Ikeda E, Yagi K, Kojima M, et al. Differentiation. 2008; 76(5): p. 495-505.
[Crossref] [Google Scholar] [PubMed]
- Zhang Q, Shi S, Liu Y, et al. J Immunol. 2009; 183(12): p. 7787-7798.
[Crossref] [Google Scholar] [PubMed]
- Liu D, Xu J, Liu O, et al. J Clin Periodontol. 2012; 39(12): p. 1174-1182.
[Crossref] [Google Scholar] [PubMed]
- Cianci E, Recchiuti A, Trubiani O, et al. Stem Cells Transl Med. 2016; 5(1): p. 20-32.
[Crossref] [Google Scholar] [PubMed]
- Shin C, Kim M, Han JA, et al. J Periodontal Res. 2017; 52(1): p. 135-146.
[Crossref] [Google Scholar] [PubMed]
- Németh K, Leelahavanichkul A, Yuen PS, et al. Nat Med. 2009; 15(1): p. 42-49.
[Crossref] [Google Scholar] [PubMed]
- Luz-Crawford P, Djouad F, Toupet K, et al. Stem Cells. 2016; 34(2): p. 483-492.
[Crossref] [Google Scholar] [PubMed]
- Ge W, Jiang J, Arp J, et al. Transplantation. 2010; 90(12): p. 1312-1320.
[Crossref] [Google Scholar] [PubMed]
- Zhou Y, Yamamoto Y, Xiao Z, et al. J Clin Med. 2019; 8(7): p. 1025.
[Crossref] [Google Scholar] [PubMed]
- Börger V, Bremer M, Ferrer-Tur R, et al. Int J Mol Sci. 2017; 18(7): p. 1450.
[Crossref] [Google Scholar] [PubMed]