Literature Review - Der Pharma Chemica ( 2024) Volume 16, Issue 5
Oral Mucositis, Incidence, Risk factors, Clinical Features, Scoring, Pathophysiology and Treatment: A Review of Literature
Ameera Kamal Khaleel*, Wisam Suyah Hassan, Hassan Salim Baqir, Muntadher Amer Jaber, Hussein Abas Jahed and Muntadher Ali ShweilAmeera Kamal Khaleel, Department of Dentistry, Al Safwa University College, Karbala, Iraq, Email: dr.ameera@alsafwa.edu.iq
Received: 09-Sep-2024, Manuscript No. DPC-24-147604; Editor assigned: 12-Sep-2024, Pre QC No. DPC-24-147604 (PQ); Reviewed: 29-Sep-2024, QC No. DPC-24-147604; Revised: 01-Oct-2024, Manuscript No. DPC-24-147604 (R); Published: 29-Oct-2024, DOI: 10.4172/0975-413X.16.5.470-475
Abstract
Cancer is a broad group of different diseases involve the unregulated cell growth in which the cells divide uncontrollably forming the malignant tumors. The management are by chemotherapy, surgery, radiation therapy or by other treatments. Oral mucositis refers to the inflammation and ulceration that occurs in the mouth and considered as a side effect of chemotherapy and/or radiotherapy treatment for malignant tumor. The aim of this study was to review the incidence, risk factors, clinical features, scoring, pathophysiology and treatment of oral mucositis. The incidence of oral mucositis is varying from patient to patient depending on the type, dose and duration of the treatment the patient receives. The risk factors are the patient-related factors (like the age, gender, racial factor, poor oral hygiene, periodontal disease, nutritional status, xerostomia, co-existing diseases, tobacco use and alcohol consumption) and the treatment-related risk factors which includes the chemotherapy risk factors (like the type of chemotherapy, dose and duration) and the radiation therapy risk factors (like the anatomical area irradiated, volume of tissue irradiated, total dose, fractionation regimen) and the concomitant chemotherapy. Oral mucositis clinically starts with redness and then progresses to the development of large and very painful pseudomembranous lesions associated with dysphagia. The non-keratinized mucosa is mostly affected than the keratinized mucosa. The pain can be so debilitating to the oral activities like swallowing, mastication, drinking and speech. Both oral and gastro intestinal mucositis may be associated with infection-related deaths and can be a dose-limiting factor for chemotherapy which affect the patient survival. A variety of scales have been used to record the severity of oral mucositis like the WHO scale and the scoring systems by national cancer institute. The WHO scale is the most widely used and includes criteria which are the presence of erythema and ulceration oral pain and the patient’s inability to eat. Regarding the pathophysiology, five phases have been identified in the development of oral mucositis and mucosal restoration. In the initiation phase tissue injury occurs following the administration of radiation or chemotherapy in which the DNA strand breakdown occur. This is followed by the primary damage response which result in the activation of several transduction pathways that activate transcription factors such as p53 and nuclear factor-κB. Signal amplification by pro-inflammatory cytokines like TNF-α can intensify the response to primary damage. The signals are amplified due to apoptosis, tissue damage and vascular permeability. This result in painful ulceration and superficial bacterial colonization. Then healing occur once the cancer therapy ends. There are only a few established treatments for oral mucositis like the topically applied cryotherapy, laser therapy, antibiotic lozenges, benzydamine hydrochloride, chlorhexidine and some herb extract mouth washes. A systemic administration of indomethacin, amifostine, growth factors or palifermin can cause a significant reduction in the severity of oral mucositis.
Keywords
Oral mucositis; Chemotherapy; Radiation therapy; Oral ulcerations
Introduction
Cancer
Cancer is a broad group of different diseases involve the unregulated cell growth in which the cells divide uncontrollably forming the malignant tumors. Then they invade the different nearby parts of the body. Cancer can spread to the distant parts of the body through the bloodstream or the lymphatic system in a process called metastasis. The causes of cancer are complex and partially understood. Many things can increase the risk of cancer like tobacco use., alcohol use, unhealthy diet like red meat, sugary drinks and refined carbohydrates, exposure to radiation, unprotected exposure to UV light, such as sunlight, environmental pollutants and infection by certain viruses like Human Papilloma Virus (HPV), hepatitis B, hepatitis C and HIV. These factors can damage genes or combine with existing genetic faults within the cells to cause the cancerous mutations. The chances of surviving the disease vary greatly by the type and location of the cancer and the extent of disease at the start of treatment. While cancer can affect people of all ages, a few types of cancer are more common in children; and the risk of developing cancer generally increases with age. In 2007, cancer caused about 13% of all human deaths worldwide (7.9 million). Rates are rising as more people live to an old age and as mass lifestyle changes occur in the developing world [1].
Types of cancer
There are over 200 types of cancer present. Several clinical terms are used for certain general types of cancer:
•Carcinoma is a malignant neoplasm which divided into adenocarcinoma, which develops in organ or gland and squamous cell carcinoma. Carcinomas are malignancies of epithelial tissue, account for 80 to 90 percent of all cancer cases. Epithelial tissue is present in the skin, as well as the covering and lining of organs and internal passageways, such as the gastrointestinal tract.
•Sarcoma is cancer of connective tissues such as muscles, bones, cartilage, fatty tissue, fibrous tissue and blood vessel. Examples of sarcomas are leiomyosarcoma, rhabdomyosarcoma, osteosarcoma, chondrosarcoma, liposarcoma, fibrosarcoma and angiosarcoma.
•Leukemia is a cancer of the bone marrow, which creates blood cells.
•Lymphoma and myeloma are cancers of the immune system.
•Melanomas are cancers that arise in the cells that make the pigment in skin.
Literature Review
Management of cancer
Chemotherapy: Chemotherapy can be administered either alone or in combination with other treatments for the prolongation of life. The function and synthesis of Deoxyribonucleic Acid (DNA) is altered by the administration of chemotherapy drugs taken orally or by injection often over a number of months. The chemotherapy drug can destroy the rapidly dividing cells in the body and slow the cell division nonspecifically. The cells mostly affected are from the gastrointestinal epithelium including the epithelium of the oral cavity and the bone marrow cells.
Chemotherapy like cyclophosphamide can directly damage the DNA to prevent the malignant cell from reproducing. Cyclophosphamide is used to treat many different cancers, including leukemia, lymphoma, Hodgkin disease, multiple myeloma and sarcoma, as well as cancers of the lung, breast and ovary [2].
Methotrexate and 5-fluorouracil are a class of drugs that interfere with DNA and RNA growth by substituting for the normal building blocks of RNA and DNA. They are used to treat leukemia, cancers of the ovary, breast and the intestinal tract. Plant alkaloids like vinblastine and etoposide are plant-derived chemicals also called mitotic inhibitors they are used to treat lung and breast cancers, myeloma, lymphoma and leukemia.
Advances in the cancer treatments have led to the increase in patient survival though the use of newly and highly toxic regimes. The administrations of these new treatments have also increased the toxicities or the side effects which are associated with their use.
Surgery: Many management options for malignant tumor depends upon the location, type and grade of the cancer. Surgery is the primary method of treatment of most solid cancers and may play a role in palliation and prolongation of survival. Surgery is also typically considered as an important part of making the definitive diagnosis by biopsy. In some types of cancer, surgery is needed only to eliminate the malignant tumor. In other types, surgery is needed to remove the entire mass along with the lymph nodes in the area.
Radiation therapy: It involves the use of ionizing radiation to either cure or improve the symptoms of cancer. It is typically used with chemotherapy or surgery or for certain types of cancer such as early head cancer may be used alone.
Other treatments: Palliative treatment is used to reduce the emotional and psychosocial distress experienced by people with malignancy and to improve the patient's quality of life. Stem cell (bone marrow) transplant can repair the diseased bone marrow with healthy stem cells. A stem cell transplant is mostly used to treat leukemia. Hormone therapy is a common treatment for cancers that may use hormones to grow and spread, such as certain types of breast cancer and prostate cancer [3-5].
Mucositis
Mucositis is a highly debilitating complication of nearly all anti-cancer therapies, including radiotherapy, chemotherapy, hematopoietic cell transplantation and even targeted therapies. Mucositis is characterized by breakdown of alimentary mucosa, initiated by the direct cytotoxic damage by the cancer treatment leading to cell death, followed by breaches in epithelial integrity and inflammation. It presenting as ulcerative lesions in the mouth, upper and lower gastrointestinal tract.
Mucositis is commonly reported by patients and considered as the most debilitating side effect of cancer treatment. The secondary complications are malnutrition, infection, cachexia, diarrhea, dehydration and renal failure. It often requires intensive and costly supportive care and often interferes with the anti-cancer therapy and may necessitate a dose reductions or treatment cessation and therefor mucositis may not only affect the patient quality of life but also the patient survival [6].
Oral mucositis
Oral mucositis is painful, debilitating and inflammatory common complication of cancer chemotherapy and/or radiotherapy to the field involving the oral cavity. The mucosa of the cheek, floor of mouth, lips and soft palate are more frequently affected by chemotherapy than keratinized mucosa such as the hard palate. Mucositis can also involve other areas of the gastrointestinal tract and can manifest as diarrhea.
Incidence: The incidence of oral mucositis is varying from patient to patient depending on the type, dose and duration of the treatment the patient receives. Mucositis has been reported to be in between 40% and 79% of patients receiving chemotherapy and between 60% and 100% of patients with neck or head malignancy and receiving radiotherapy and 92% of patients receiving both radiation therapy and chemotherapy. But in patients undergoing bone marrow transplants the incidence was seen 76% to 100% of the patients with mild to moderate severity of oral mucositis and between 66% and 76% of patients developing severe oral mucositis. In patients that receiving a high dose of myeloablative therapies, the incidence of oral mucositis is nearly 100% [7].
Risk factors
Patient-related factors: Age, gender, racial factor, poor oral hygiene, periodontal disease, nutritional status, xerostomia, co-existing disease, tobacco use and alcohol consumption have a major influence on the severity and duration of oral mucositis. The younger patient tends to develop oral mucositis more than the older patients because of a more rapid turnover of the basal cells in the oral mucosa of the younger patients. The elderly patients are also thought to be with an increased risk of developing oral mucositis due to the compromised tissue recovery caused by the decline in stem cell reserves.
A significantly greater risk of oral mucositis has been found in women than men and appears more severe and lasts longer. Others study found no sexual predilections to chemotherapy induced oral mucositis. American patients treated with 5-fluorouracil for colon cancer have been found to experience less oral mucositis than Caucasian patients. But McCollum, et al found that there are no racial predilections to chemotherapy induced oral mucositis [8].
Intensive oral hygiene care is important for reduction in the frequency of oral mucositis. The extent and composition of the oral micro flora in patients with poor oral hygiene increase the susceptibility to oral mucositis.
Pre-existing conditions such as gingivitis, periodontal disease and dental carries are likely to cause a higher incidence of oral mucositis. Wearing a dental appliance or the presence of a sharp teeth has been reported to be a possible risk factor due to a possible continuous trauma.
Patients report that oral irritants like alcohol, smoking, spicy or hot foods can cause irritation and increase the mucosal damage and pain levels. Patients who have smoking may be at a higher risk for developing mucositis because the smoking can affect the healing potential of the oral mucosa. Other study found that patients with poor nutritional status are at a higher risk for developing the oral mucositis then patients with good oral hygiene.
Treatment-related risk factors: Treatment-related risk factors that increase the probability of developing oral mucositis are:
Chemotherapy risk factors like the type of chemotherapy, dose and duration.
Radiation therapy risk factors like the anatomical area irradiated, volume of tissue irradiated, total dose, fractionation regimen and concomitant chemotherapy.
The type of chemotherapy affecting DNA synthesis exhibit the most pronounced effects. Prolong administration of a low doses of chemotherapy was found to be associated with an increased risk of developing oral mucositis and a high dose of chemotherapy was seen associated with a greater risk of developing oral mucositis [9].
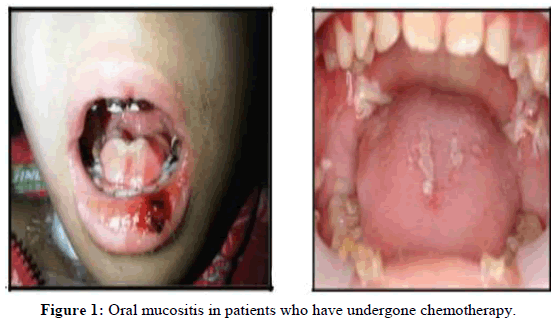
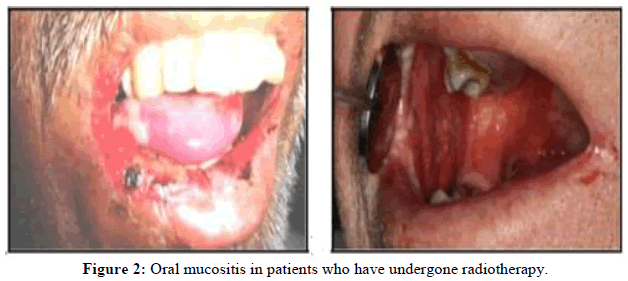
Clinical features of oral mucositis: Oral mucositis may be very painful and can significantly affect the nutrition and mouth care. It starts with redness and then progresses to the development of large and very painful pseudomembranous lesions associated with dysphagia. The nonkeratinized mucosa is mostly affected than the keratinized mucosa. Figures 1 and 2 showing oral mucositis following chemotherapy and radiotherapy.
Pain from oral mucositis is the most common complication and its management is very difficult. Topical therapies are needed, put some patients may need a systemic therapy in a more serious case. The severity of pain correlates with the ulcerative phase of oral mucositis. This pain of oral mucositis can be so debilitating to the oral activities like swallowing, mastication, drinking and speech. Patients can become dehydrated and malnourished and hospitalization with parenteral administration of fluids, analgesics and total parenteral nutrition is warranted.
Infections associated with the oral mucositis can cause a life-threatening systemic sepsis during the periods of immunosuppression. Some cases of oral mucositis have been correlated with systemic infection. In patients receiving chemotherapy for lymphoma or for solid tumors, the rate of systemic infection in patients with mucositis was more than that in patients without mucositis and was proportional to the severity of mucositis.
Neutropenia can enhance the degree of oral mucositis: The more serious neutropenia was seen associated with a more serious the oral mucositis. Both oral and gastro intestinal mucositis may be associated with infection-related deaths and can be a dose-limiting factor for chemotherapy which affect the patient survival [10].
Scoring oral mucositis: The oral mucositis score is used to measure the toxicity of a particular drug or regimen and to determine the efficacy of the new treatments for the condition. A variety of scales have been used to record the severity of oral mucositis. The commonly used scoring systems can be divided into two categories: those that document the general appearance of the oral cavity and anatomical distribution of the mucosal lesions and those that also assess oral health, function and patient morbidity factors. The WHO scale is the most widely used and includes criteria which are the presence of: erythema and ulceration oral pain and the patient’s inability to eat. This scale combines both objective and subjective measures of oral mucositis as seen in Table 1. The National Cancer Institute (NCI) Common Terminology Criteria for Adverse Events (CTCAE) includes a separate objective and subjective scales for oral mucositis as seen in Table 2 [11].
| Grade | Factors |
|---|---|
| Grade 0 | None |
| Grade 1 (mild) | Oral soreness, erythema |
| Grade II (Moderate) | Oral erythema, ulcer, solid diet tolerated |
| Grade III (Severe) | Oral ulcers, liquid diet only |
| Grade IV (life threatening) | Oral alimentation impossible |
Table 1: Commonly used oral mucositis scoring systems (WHO: World Health Organization).
| Grade | Factors |
|---|---|
| Grade 1 | Erythema of the mucosa |
| Grade 2 | Patchy ulcerations or pseudomembranes |
| Grade 3 | Confluent ulcerations or pseudomembranes; bleeding with minor trauma |
| Grade 4 | Tissue necrosis; significant spontaneous bleeding; life-threatening consequences |
| Grade 5 | Death |
| Grade 1 | Minimal symptoms, normal diet |
| Grade 2 | Symptomatic but can eat and swallow modified diet |
| Grade 3 | Symptomatic and unable to adequately aliment or hydrate orally |
| Grade 4 | Symptoms associated with life-threatening consequences |
| Grade 5 | Death |
Table 2: Oral mucositis scoring systems by National Cancer Institute (NCI) Common Terminology Criteria for Adverse Events (CTCAE) version 3.0.
Pathophysiology
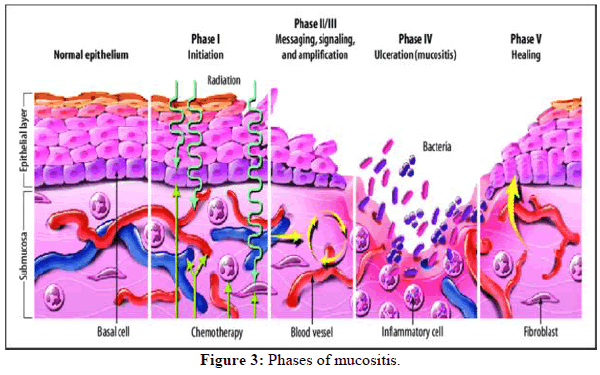
Oral mucositis is a complex interaction of the epithelium with the submucosa in response to chemotherapy administration. Five phases have been identified in the development of oral mucositis and mucosal restoration and considered as a useful mode for understanding the chemotherapy induced oral mucositis. Figure 3 shows the phases of this model which are:
Initiation phase: This stage of tissue injury occurs following the administration of radiation or chemotherapy. DNA strand breakdown result in a direct cellular injury that targets cells in the basal epithelium as well as cells in the submucosa with generation of reactive oxygen species. Although the epithelium seems clinically normal at this stage, but a series of molecular reactions in the connective tissue occur before clinically manifesting on the epithelium.
Primary damage response: The DNA strand breakdown result in the activation of several transduction pathways that activate transcription factors such as p53 and nuclear factor-κB (NF-κB) which potentially have an effect on mucosal toxicity (SonisThe upregulation of genes due to chemotherapy or radiation therapy can results in the production of pro-inflammatory cytokines like TNF-α, IL-1β and IL-6 within the mucosa and their presence stimulates the early damage to connective tissue and results in basal cell death.
Signal amplification: Signals are amplified due to apoptosis, tissue damage and vascular permeability. Pro-inflammatory cytokines can intensify the response to primary damage. TNF- α is an efficient activator of NF-κB. This complex pathway ultimately results in activation of caspase 3 and cell death and also amplify the primary damage that is initiated by radiation or chemotherapy [12].
Ulceration: The ulcers tend to be deep, irregular in shape, with extremely severe pain that are prone to superficial bacterial colonization. These ulcerations serve as portals of entry for the different microorganisms which often lead to bacteremia and sepsis. These colonizing bacteria can activate the infiltration of mononuclear cells to release additional pro-inflammatory cytokines and potentiates the tissue injury.
Healing: Mucositis is an acute phenomenon that is self-resolving once the cancer therapy ends. The epithelial cells surround the ulcer begin to proliferate and migrate into the wounded bed and the tissue will start to form layers and the normal oral micro flora will be re-established. The healing of these ulcerations depends on several factors such as the presence of systemic diseases, host immunity or the presence of opportunistic infections.
Discussion
Treatment of oral mucositis
Management of oral mucositis has been largely palliative to date, like nutritional support, pain control, palliation of dry mouth and oral decontamination, but targeted therapeutic interventions are now being developed. There are only a few established treatments for oral mucositis and their effectiveness is variable. The treatment must not diminish the tumoricidal effect of the antineoplastic treatment.
Locally applied non-pharmacological methods: Studies which evaluated the cryotherapy noted a benefit in patients who chewed on ice for thirty minutes before each chemotherapy infusion. It causes a local vasoconstriction and temporarily reduces the blood flow during the time of peak serum drug concentrations.
Lasers have been reported to produce analgesia and wound healing. It was documented that it can decrease inflammation, edema and pain in laser treated tissues. Fekrazad and Chiniforush also found that low-level laser therapy is a safe approach for management and prevention of oral mucositis.
Topically applied pharmacological methods: Chlorhexidine exhibit anti-bacterial and anti-mycotic activities and is considered as one of the most commonly used mouthwashes. Eilers study found that it cannot decrease the severity of oral mucositis. Homemade salt solutions have been recommended by dentists only to improve dental hygiene. Local pain therapies like lidocaine have a limited benefit as the lidocaine wears away after only a few minutes. Sedighi, et al., demonstrates that the topically applied honey in the oral cavity can reduce the severity of chemotherapy induced mucositis. Chamomile extract have anti-inflammatory effect and can promote granulation tissue formation and mucosal healing.
Benzydamine hydrochloride is a drug which has analgesic, antimicrobialand anti-inflammatory activities and has been used as a mouthwash for prevention or treatment of oral mucositis. In patients with head and neck cancer, there is good evidence that benzydamine hydrochloride mouthwash is effective in decreasing the symptoms of radiation induced mucositis or chemotherapy induced mucositis. Al-Jaf, et al. and Ahmed, et al., found that olive leaf extract as a local treatment was more effective in decreasing the severity of oral mucositis when compared to benzydamine hydrochloride.
Antibiotic lozenges have been widely recommended to reduce oral infections associated with mucositis. Antifungal agents like nystatin and clotrimazole are effective local antifungal agents. Antiviral therapies such as acyclovir, are effective treatments for viral infection in the oral cavity. Treatment of infections, however, does not clear oral mucositis [13].
Sucralfate is a basic aluminum salt of sucrose sulfate and when contacted with ulcerated mucosa can promotes the local production of prostaglandins, which acts as a cytoprotectant stimulating epithelial proliferation, migration and blood flow.
Retinoid is known induce epithelial growth and enhance the mucosal resistance to toxicities and decrease the severity of mucositis induced by chemotherapy and radiotherapy. Topical vitamin E can interfere with the inflammatory damage create by radiotherapy and chemotherapyand the clinical trials have shown significant improvement in reducing severity of oral mucositis.
Systemically applied non-pharmacological methods: Al-Refai, et al., found that green tea extract at a concentration of 40 mg/kg/day can produce a protection against methotrexate induced oral mucositis by its anti-apoptotic and antioxidant activitiesand can be used as a protective natural product to oral mucosa against methotrexate induced cytotoxicity [14].
Systemically applied pharmacological methods: A randomized controlled trial demonstrating that the systemic administration of indomethacin can cause a significant reduction in the severity of radiotherapy induced mucositis.
Amifostine which is a cytoprotective agent can also promotes repair of damaged DNA. Infusions of immunoglobulin G can regulate the function of T effecter cells with down regulation of the inflammatory cytokine.
Growth factors: Growth factors that may have an impact on mucositis are Granulocyte-Colony Stimulating Factor (G-CSF) and Granulocyte Macrophage Colony Stimulating Factor (GM-CSF) and Keratinocyte Growth Factor (KGF).
G-CSF and GM-CSF may reduce oral mucositis by accelerating neutrophil recovery and stimulate the regeneration of oral mucosa and helping in prevention and treatment of chemotherapy induced mucositis. Other study indicates that palifermin can prevent and reduce oral mucositis in patients undergoing 5-fluorouracil chemotherapy. Palifermin reduced the incidence of grade 2, 3 and 4 from 78% to 32% and decreased the duration of severe mucositis [15].
Conclusion
Oral mucositis is painful, debilitating and inflammatory common complication of cancer chemotherapy and/or radiotherapy to the fields involving the oral cavity. The incidence of oral mucositis is varying from patient to patient depending on the type, dose and duration of the treatment the patient receives. Clinically, oral mucositis starts with redness and then progresses to the development of large and very painful pseudomembranous lesions associated with dysphagia. The WHO scale for the oral mucositis is the most widely used and includes criteria which are the presence of: erythema and ulceration, oral pain and the patient’s inability to eat. Regarding the pathophysiology, five phases have been identified, the initiation phase, primary damage response, signals amplification, painful ulceration, then healing occur once the cancer therapy ends. There are only a few established treatments for oral mucositis like the topically applied cryotherapy, laser therapy, antibiotic lozenges, benzydamine hydrochlorid chlorhexidine and some herb extract mouth washes. A systemic administration of indomethacin, amifostine, growth factors or palifermin can cause a significant reduction in the severity of oral mucositis.
References
- Ahmed KM, Talabani N, Altaei T. Pharmaceut Anal Acta. 2013; 4(9): p. 1-8.
- Allana A, Shamsi U, Rashid Y, Khan FR, Rozi S. Plos one. 2024; 19(4): p. 0295456.
[Crossref] [Google Scholar] [PubMed]
- Al-Refai AS, Ali AB, Kamal KA. J Cytol Histol. 2014; 5(3): p. 1-7.
- Al-Taie A, Al-Shohani AD, Albasry Z, et al. J Pharm Bioallied Sci. 2020; 12(2): p. 94-101.
[Crossref] [Google Scholar] [PubMed]
- Anand P, Kunnumakara AB, Sundaram C, et al. Pharm Res. 2008; 25(9): p. 2097-2116.
[Crossref] [Google Scholar] [PubMed]
- Avritscher EB, Cooksley CD, Elting LS. Semin Oncol Nurs. 2004; 20(1): p 3-10.
[Crossref] [Google Scholar] [PubMed]
- Bamba Sandoh A, Yasui H, et al. J Gastroenterol. 2003; 38: p. 548-554.
[Crossref] [Google Scholar] [PubMed]
- Bellm LA, Epstein JB, Rose-Ped A, et al. Support Care Cancer. 2000; 8: p. 33-39.
[Crossref] [Google Scholar] [PubMed]
- Bolwell BJ, Kalaycio M, Sobecks R, et al. Bone Marrow Transplant. 2002; 30(9): p. 587-591.
[Crossref] [Google Scholar] [PubMed]
- Braguês R, Marvão MF, Correia P, et al. Cancers. 2024; 16(8): p. 1548.
[Crossref] [Google Scholar] [PubMed]
- Brown TJ, Gupta A. JCO Oncol Pract. 2020; 16(3): p. 103-109.
[Crossref] [Google Scholar] [PubMed]
- Camejo N, Castillo C, Tambasco C, et al. World J Surg Oncol. 2023; 14(4): p. 300.
[Crossref] [Google Scholar] [PubMed]
- Cassileth BR, Deng G. Oncologist. 2004; 9(1): p. 80-89.
[Crossref] [Google Scholar] [PubMed]
- Chansky K, Benedetti J, Macdonald JS. CA Cancer J Clin. 2005; 103(6): p. 1165-1171.
[Crossref] [Google Scholar] [PubMed]
- Correa ME, Cheng KK, Chiang K, et al. Support Care Cancer. 2020; 28: p. 2449-2456.
[Crossref] [Google Scholar] [PubMed]