Mini Review - Der Pharma Chemica ( 2021) Volume 13, Issue 6
Methotrexate model of Hepatotoxicity: A Review
Deepika Bhatia* and Dr Pradeep GoyalUniversity institute of pharmaceutical sciences, Chandigarh University, Gharaun, India
Deepika Bhatia, University institute of pharmaceutical sciences, Chandigarh University, Gharaun, India, Email: BHATIA.DEEPIKA89@GMAIL.COM
Received: 24-Mar-2021 Accepted Date: Jun 23, 2021 ; Published: 30-Jun-2021
Abstract
The liver is an important organ for maintenance of body general function and homeostasis. In addition to its role in the digestive process, it is important to detoxify unwanted substances. There are many varieties of drugs and chemicals are used to shows a toxic effect on liver e.g. ccl4, Peracetamol, Glactosamine, Methotrexate and many more at different dose. In this review we are going to discuss the toxic dose of methotrexate causes hepatotoxicity. Methotrexate (Mtx) is a antagonist of folic acid and also a cytotoxic agent that is responsible to inhibit cellular growth. It is used in many clinical symptoms i.eleukemia, lymphomas etc. The present overview summarizes some of the basic concepts involved in hepatotoxicity, their preclinical evaluation methods and some hepatotoxic models based upon dose.
Keywords
Hepatotoxicity, Methotrexate, Mechanism, Hepatotoxic model.
Introduction
Hepatotoxicity is a major cause of mortality and mobility now days. It is mainly occurs by the inorganic compounds, organic agents and synthetic drugs. These inorganic ad organic agents and synthetic drugs which undergo metabolism in the liver and produces free radicals in the liver which causes damage to liver [1]. Drugs are very comman reason responsible for liver injury. Approximately 1000 drugs, herbal drugs have been report to root injury in liver, and drugs account for 20-40% of hepatic failure. Almost 75% of the idiosyncratic drug reactions end up to transplantation of liver or some causing time death. Drug-induced hepatic injury is the most common cause for taking out of an permitted drug from market [2,3].
Methotrexate
Methotrexate (MTX), Previously was also named as anamethopterin, it is effective chemotherapy drug and also an immune suppressing agent used to cure various illness i.e. cancer, autoimmune diseases, ectopic pregnancy, and for medical abortions.[4,5] the various types of cancer include breast cancer, lung cancer, lymphoma, gestational trophoblastic disease, and osteosarcoma. [6,7].
It is an agent which is antifolate and antimetabolite generally used to treatment psoriasis and arthritis. Methotrexate is also used in other autoimmune diseases in the modified form [8]. Methotrexate acts by inhibiting metabolism of folate and blockage of dihydrofolic acid reductase and cause inhibit the synthesis of purines or pyrimidines and lower down the synthesis of DNA and RNA. When it is given in high dose as a intravenous route, methotrexate can also cause acute elevations of the enzymes of serum, and long term use elevations in serum liver enzymes mild and high and cause chronic liver injury [9,10].
Methotrexate is belonging to the class of antimetabolites. This treatment shows the growth of cancer causing cells. Methotrexate also used to treats psoriasis [11].
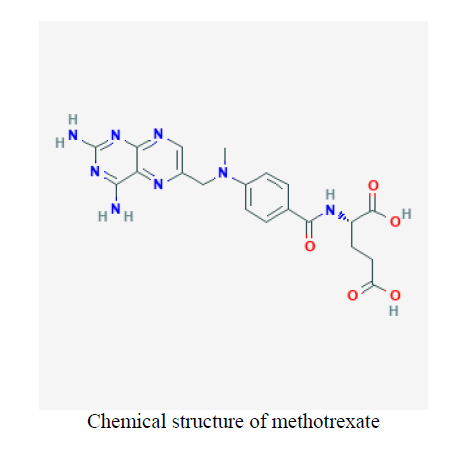
Chemical structure
History
Methotrexate was firstly introduced in 1947, and originally in beginning used to treat cancer. In 1956 it is first used to cures metastatic cancer. Methotrexate is the most prescribe medicine in the U.S this drug has higher than six hundred lakh prescriptions in 2017 [12,13].
Mechanism of action
Methotrexate entered into tissues and got converted to folylpolyglutamate to methotrexate polyglutamate [14]. Mechanism of action of methotrexate is acting on inhibition of enzymes i.e. dihydrofolate reductase, thymidylate synthase, aminoimidazole caboxamideribo nucleotide transformylase (AICART), and amidophosphoribosyl transferase Inhibtion of nucleotide synthesis inhibit the cell division [15,16].
Hepatic injury introducing with methotrexate is responsible for direct toxicity, via inhibition of RNA and DNA synthesis in the liver by producing cellular arrest. This therapy has been proved to raise hepatic stellate cell numbers, but the mechanism by which fibrosis occure has not been clearly explain [17,18].
Dose related study of methotrexate
Recent study shows in Wistar rats for the development of an animal model of drug methotrexate causing hepatotoxicity. Animal had been treated with different dosage of methotrexate in i.e. 100, 150, 200 and 300 micrograms/kilogram each day doses for different interval in oral. The higher dose 300 micrograms/kilogram in day had formed systemic toxicity in animals. The animals required being sacrifice early, and toxicity of liver was not been proved. The minor doses of methotrexate has been allowed for long durations of time and cause hepatotoxicity in these five rats treated with 200 micrograms/kilogram in one day, four rats receiving 150 micrograms/kilogram in each day and other group of five rats on 100 micrograms/kg/day. In every treated group in the hepatic damage ranges in harshness from focal necrosis to necrosis of zone [19-21]. Other group of five rats treated with 100 micrograms/kg/day dose of methotrexate treated for 6 weeks causes liver injury shows crucial necrosis, lysis of cell and also cause puffy Kupffer cell and in totalling three animals(rat) shows early on hepatic fibrosis in liver by oral route of administration cause hepatotoxicity.
Despite studies by scientists over the years, the conventional method of vaccine production against Campylobacter in poultry has not led to the development of vaccine in terms of immunogenicity. It is important to intensify efforts to test and validate new vaccine antigens, hence, reverse vaccinology is a suitable strategy to this end [5].
There are many other models of hepatotoxicity with different dose and at different time interval with the use of animals I.e. rat, mice, rabbit as discuss in table below:
| Sr no | Animal used | Dose | Time | Reference |
|---|---|---|---|---|
| 1 | rat | 300 ug/kg/day 200 ug/kg/day 100 ug/kg/day (p.o) |
4weeks | 22 |
| 2 | Albino rats | 20 mg/kg/ip | single dose | 23 |
| 3 | Albino Mice | 1750 mg/kg | 1 days | 24 |
| 4 | Rabbits | 20 mg/kg/ip | 3 days | 25 |
| 5 | Wistar rats | 100 µg/kg | 45 days | 26 |
| 6 | Sprague-dawley rats | 20 mg/kg | single dose | 27 |
| 7 | Wistar rats | 20 mg/kg | 12 days | 28 |
| 8 | Wistar rats | 20 mg/kg | 5 days | 29 |
| 9 | Wistar rats | 20 mg/kg | single dose | 30 |
| 10 | Wistar rats | 20 mg/kg | 10days | 31 |
| 11 | Wistar rats | 20 mg/kg | 5days | 32 |
| 12 | Wistar rats | 20 mg/kg | 7days | 33 |
| 13 | Wistar rats | 20 mg/kg | 10days | 34 |
References
- Methotrexate. The American Society of Health-System Pharmacists, 2016.
- Gurfateh Singh, Deepika Bhatia and Harikumar SL. Der Pharma Chemica, 2015. 7(4): p. 164-168
- Sneader W. Drug Discovery: A History, 2005.
- Today's anti-cancer tools are ever better wielded. The Economist, 2017.
- World Health Organization. (2019). World Health Organization model list of essential medicines:
- Clegg DO, Furst DE, Tolman KG. J Rheumatol, 1989. 16: p. 1123–6.10.
- Weinblatt ME, Dixon JA, Falchuk KR. Arthritis Rheum, 2000. 43: p. 2609–11.
- Colsky J, Greenspan EM, Warren TN. AMA Arch Pathol, 1955. 59: p. 198–206.
- Hutter RVP, Shipkey FH, Tan CTC et al., Cancer, 1960. 13: p. 288–307.
- Ryan TJ, Vickers HR, Salem SN et al., J Dermatol, 1964. 76: p. 555–64.
- Hersh EM, Wong VG, Henderson ES et al., Cancer. 1966. 19:600–6.
- Talerman A, Thompson RB. J ClinPathol, 1966. 19: p. 81–2.
- Fry L. Br J Dermatol. 1966. 78: p. 282–8.
- Custer P, Freeman-Narrod M, Narrod SA. J Natl Cancer Inst, 1977.58: p. 1011-101
- Coe RO, Bull FE. JAMA, 1968. 206: p. 1515–20.
- Auerbach R. JAMA, 1969. 208: p. 155.
- Roenigk HH Jr, Fowler-Bergfeld W, Curtis GH. Arch Dermatol, 1969. 99: p. 86–93.
- Dahl MG. Br J Dermatol, 1969. 81: p. 465–7.
- Dubin HV, Harrell ER. JAMA, 1969. 210: p. 1104.
- Epstein EH Jr, Croft JD Jr. Arch Dermatol, 1969. 100: p. 531–4.
- McDonald CJ, Bertino JR. Arch Dermatol, 1969. 100: p. 655–68.



