Review Article - Der Pharma Chemica ( 2022) Volume 14, Issue 5
Ikk-Alpha Role in Colorectal Cancer - A Contemporary Anti-Cancer Target For Prioritising Colorectal Cancer Research
Anitha L* and Sinoy SugunanAnitha L, School of Pharmacy, GITAM Deemed to be University, Hyderabad Campus, Rudraram, Sangareddy, Telangana 502329, India, Email: aloknath@gitam.in
Received: 17-Apr-2022, Manuscript No. dpc-22-61071; Editor assigned: 20-Apr-2022, Pre QC No. dpc-22-61071; Reviewed: 04-May-2022, QC No. dpc-22-61071; Revised: 07-May-2022, Manuscript No. dpc-22-61071; Published: 14-May-2022, DOI: 10.4172/0975-413X.14.5.28-33
Abstract
The IKK-alpha, B kinase, or IKK enzyme complex is involved in the propagation of the cellular response to inflammation. The upstream NF-B signal transduction cascade includes the IB kinase enzyme complex. By masking the nucleus localization signals (NLS) of NF-B proteins and keeping them sequestered in an inactive state in the cytoplasm, the IKB alpha (inhibitor of nuclear factor kappa B) protein inactivates the NF-B transcription factor. IKK phosphorylates the inhibitory IB protein in particular. The separation of IB from NF-B occurs as a result of this phosphorylation. Now that NF-B is liberated, it migrates into the nucleus and activates at least 150 genes, some of which are anti-apoptotic. FL-IKK must be proteolytically cleaved into p45-IKK in order to avoid the formation of p45-IKK.The proteolytic cleavage of FL-IKK into p45-IKK is essential for colorectal cancer cells to avoid apoptosis in vitro and to maintain tumour development in vivo. As a result, inhibiting IKK-alpha is a promising therapeutic target for colorectal cancer. The purpose of this review is to look at the involvement of IKK-alpha in colorectal cancer.
Keywords
IKK- Alpha; Cytokine; Colorectal cancer; IKK-alpha B kinase; Anticancer; Small molecules; In-vitro and In-vivo
Introduction
Inflammation and cancer have been studied together and even inflammatory cytokines are believed to have a role in colon carcinogenesis by inducing neoplastic transformation. Recent investigations have shown that NF-kappaB [1] signalling pathway is activated in many tumor cells such as colon cancer. In these studies, it has been reported that NF-kappaB could act both as an oncogene and tumor suppressor depending on its activation state. The inflammatory cytokines activate NF-kappaB in epithelial cells which increase its transcriptional activity through inhibition of its phosphorylation by I kappa B kinase alpha (IKKα) [2]. Thus, targeting inhibitors to inhibit NF kappa B pathway might provide new options to treat chronic inflammation related diseases including cancer. This review focuses on highlighting recent advances regarding IKK-alpha [3-6] as an important therapeutic target against colorectal cancer (CRC) with special emphasis on its mechanism of action, structure and recent advances in anti-cancer drug discovery programs. Finally, future directions and perspectives will be discussed based on recent developments in small molecule inhibitor research against IKK-alpha [7-9].
Nuclear factor kappa B (NF-κB) is known as a key transcription factor that plays crucial roles in regulating cell survival, apoptosis, and proliferation and differentiation processes. As one of several proteins comprising different subunits encoded by different genes located at various locations within chromosome 5q31 region encoding NF-κB complex [10 - 11]. There are five distinct members from four families: RelA/p65 (also known as p50), cRel/p52, RelB/p100, and NFKBIA/p100 or p105 protein which function to form either homo or heterodimers following their assembly into complexes.
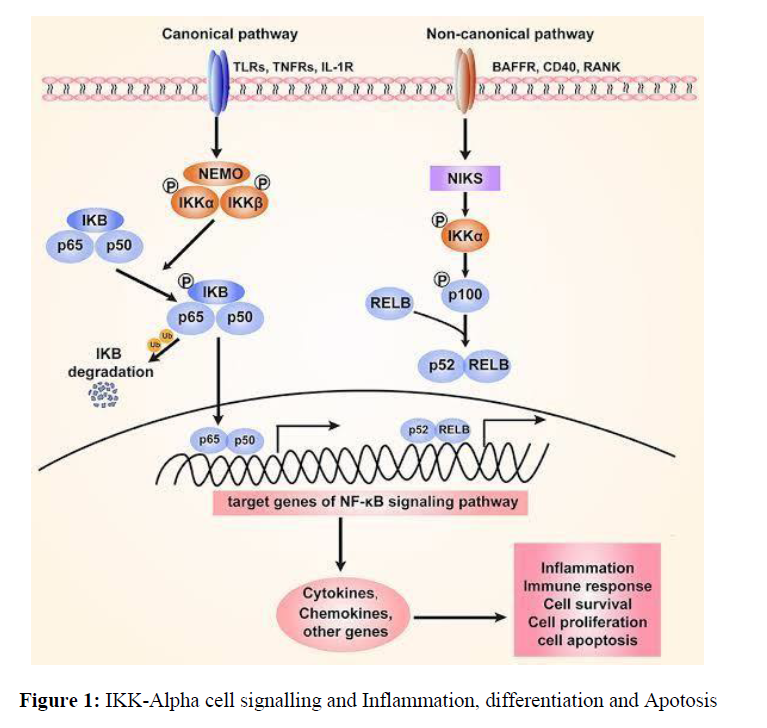
Activation of a specific transcription factor, nuclear factor (NF)-κB, has been shown to be involved in carcinogenesis. One important regulatory cascade involves NF-κB signalling and inflammatory cytokines (primarily IL-1, TNF alpha and IFN gamma). Activation of NF-κB occurs as a result of conformational changes involving its inhibitory kinase (IKK) complex [12]. This process is tightly regulated by inhibitory proteins including IκBs that mask phosphorylated serine residues located on NF-kB subunits [13-16]. The unrepressed nuclear translocation results in activation of DNA binding activity with subsequent induction and regulation of proinflammatory gene expression via target genes containing NFKB response elements in their promoter regions. In addition, activated NF-κB also regulates many other cellular processes such as cell survival, proliferation and apoptosis through direct or indirect effects on various target genes. In addition to being activated by cytokines, NF-κB [17-19] can also be activated by reactive oxygen species (ROS), ultraviolet light and ionizing radiation. These pathways converge at several points resulting in common downstream targets that are responsible for inducing inflammatory (Figure 1) responses which may have implications in colorectal cancer development.
Inhibition of IKK-alpha: Because of these positive effects of IKKα inhibition, it was hypothesized that targeting the upstream regulator(s) could provide novel therapeutic strategies for treating cancer especially colon cancer which is one of most prevalent cancers worldwide [20-21].
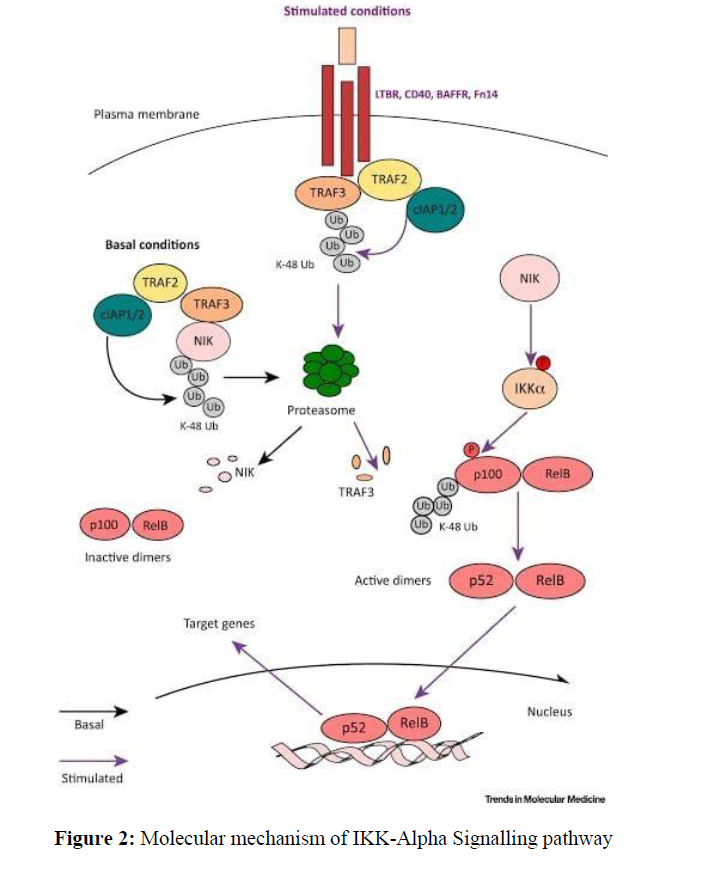
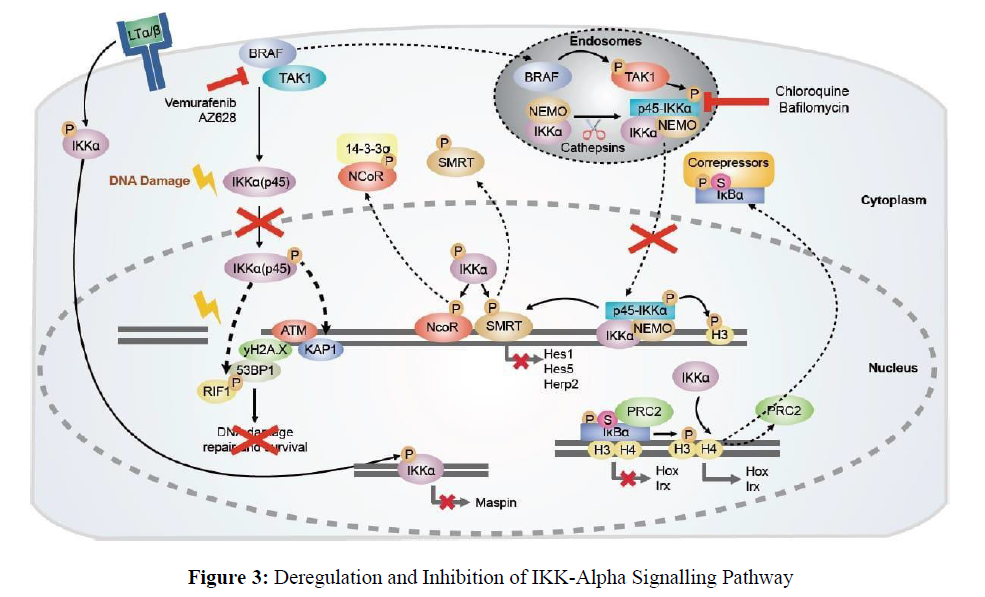
Molecular mechanism of Ikb -Kinases
The NF-kB family has a unique architecture. The NF-kB subunits can be divided into two domains: an N-terminal regulatory domain and a C terminal transactivation domain [22]. The N terminal domain folds as an amphipathic helix and serves to bind p50/p65, RelB and cRel via hydrophobic interactions with their unstructured tails [23-26]. This binding causes their dimerization, which leads to interaction with IkB via its tandem dimerization repeats. Binding to IkB also affects downstream signaling pathways (Figures 2,3) by causing sequestration of IkB in cytoplasmic aggregates, inactivating its inhibitory function. Phosphorylation is only possible on serine residues within both transactivation and regulatory domains. The phosphorylation sites are highly conserved among all members of NF-kB family but vary among different species. For example, mammalian cells contain three sites that are located at positions S32/S36 (RelA), S177 (NFKB1) and S181 (NFKB2) [27-30]. These phosphorylated residues serve as docking sites for various protein kinases such as MAPKs, PKC or IKKs. In addition to phosphorylation, these kinases may also be involved in ubiquitination and sumoylation events. Ubiquitination appears to play a role in regulating NF-kB activity during apoptosis and inflammation. Sumoylation acts as a posttranslational modification mechanism for regulating DNA binding activity of some transcription factors including NF-kB [31]. As mentioned earlier, activation of NF-kB requires not only phosphorylation but also translocation from cytosol to nucleus. It is still unclear how activated IKK alpha triggers translocation process since it does not possess any known nuclear localization signal sequences.
Current strategy for Targeting IKK-alpha for Colorectal Cancer
As activated NF-kappaB signalling has been found to promote colorectal cancer by activating tumor growth and angiogenesis, targeting NF-kappaB has been recently focused in developing new anti- cancer drugs. It has been reported that high expression level of interleukin 1 beta (IL1beta) can activate NF-kappaB signalling pathway and consequently promote colorectal cancer development. IL1beta is mainly released from macrophages (M2 phenotype) in tumor microenvironment. Inhibiting IL1beta/NFkappaB pathway may suppress or even reverse tumor growth. So far, various approaches have been investigated for inhibiting IL1beta/NFkappaB pathway including pharmacological intervention such as use of neutralizing antibodies against IL1beta or its receptor.
However, these strategies need further investigation to evaluate their effectiveness in vivo before clinical application. Therefore, a novel strategy should be developed to target IKK-alpha activity which is a critical upstream regulator of NF-kappaB activation in colon cancer cells. The current study was aimed at evaluating whether siRNA mediated knockdown of IKK-alpha could effectively inhibit NF-kappaB activation and reduce cell proliferation in colon cancer cells. We also wanted to determine if administration of IKK-alpha siRNA could inhibit tumor growth in mice xenograft model. Results showed that IKK-alpha siRNA treatment efficiently reduced both basal and IL1beta induced NF-kappaB activation as well as cell proliferation in colon cancer cells. Moreover, administration of IKK-alpha siRNA significantly inhibited tumor growth in mice xenograft model. Our results suggest that down regulation of IKK-alpha expression using small interfering RNA technique might provide an effective approach for treating patients with advanced stage colorectal cancer by reducing tumor burden and improving patient survival rate.
Review about Currently Available Small molecules for inhibition of IKK-alpha
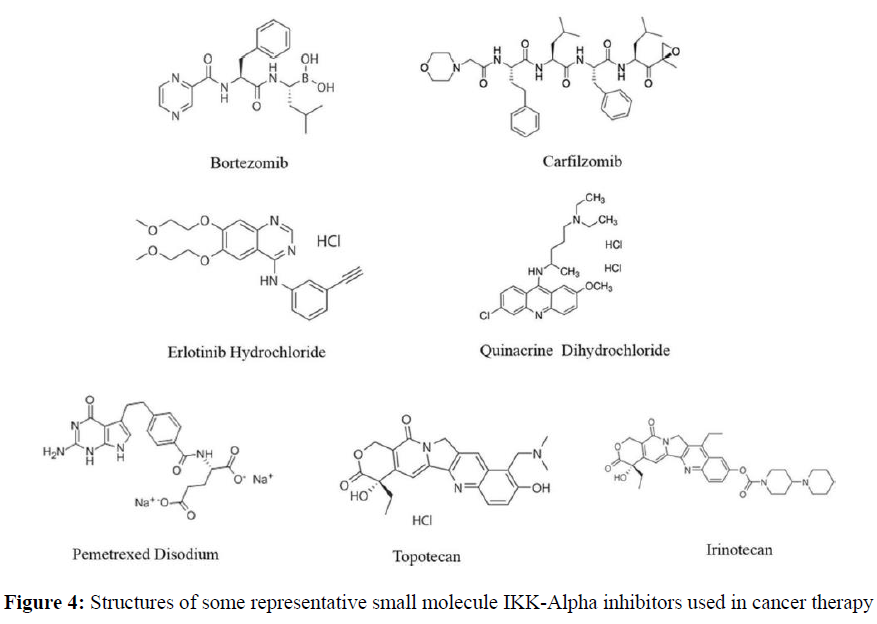
The role of c-IRAK and IKK-alpha in colorectal cancer is still largely unknown. Current evidence indicates that high levels of c-IRAK are associated with an unfavourable prognosis in CRC patients, but more studies are needed to determine if there is a correlation between IRAK and colorectal cancer progression. Specifically, whether IRAK inhibitors (Figure 4 and Table 1) could be used to treat colorectal cancer needs further investigation. There are also very few data available on interactions between IRAK1 and NFkB or interleukin 6, making it difficult to predict their relationship. Further research should focus on providing answers regarding how genetic polymorphisms affect IRAK expression and whether they predict a patient’s response to treatment. Studies involving animal models would also help us understand IRAK function better, as well as clarify its involvement in tumorigenesis. In addition, researchers should investigate whether inhibiting IRAK1 can improve chemotherapeutic agents by reducing inflammation and proliferation caused by cytokines such as IL6. Since IL6 may be involved in promoting colorectal cancer cell growth, inhibiting its effects may increase efficacy of chemotherapy drugs. Overall, more studies are needed to understand how inhibition of IRAK affects inflammatory pathways and cell signalling pathways leading to apoptosis (programmed cell death). As we begin to gain a better understanding of these processes, we will have greater insight into developing effective therapeutic strategies against colorectal cancer.
| Compound name | Type | Institute/ Company / Brand name | Target(s) | FDA approved/ phase of development |
|---|---|---|---|---|
| Bevacizumab [32] | Recombinant humanized monoclonal antibody | Avastin | VEGF via NF-κB | FDA approved |
| Bortezomib [33-35] | Proteosome inhibitor | Velcade | NF-κB | FDA approved |
| Doxorubicin Hydrochloride [36] | Antineoplastic agents | Adriablastin | NF-κB | FDA approved |
| Carfilzomib [37] | Proteosome inhibitor | Kyprolis | NF-κB | Phase I/II trial |
| Erlotinib Hydrochloride and QuinacrineDihydrochloride [38] | Tarceva - 9- aminoacridines | Seidman Cancer Center | NF-κB | Phase I |
| Bortezomib and Pemetrexed Disodium [39] | Proteosome inhibitor - multi- targeted Antifolate | University of California | NF-κB | Phase I/II trial |
| Bortezomib and Topotecan [40] | Proteosome inhibitor – Topoisomerase Inhibitor | National Cancer Institute | NF-κB and Topoisomerase | Phase I |
| Bortezomib and Gemcitabine [41] | Proteosome inhibitor – Antineoplastic agents | Masonic Cancer Center | NF-κB | Phase I |
| Carfilzomib and Irinotecan [42] | Proteosome inhibitor – Topoisomerase Inhibitor | Cancer Research and Biostatistics Clinical Trials Consortium | NF-κB and Topoisomerase | Phase I/II trial |
| *Inhibitor clinical development information current as of Feb 2020 from the United States National Institutes of Health registry clinical trials and National Institute of health [Available from: http:// www.clinicaltrials.gov and https://www.cancer.gov/about-cancer/treatment/clinical-trials] | ||||
In-vitro screening methodology for IKK-alpha for colorectal cancer
Understanding colorectal cancer is important in understanding an array of diseases which are targeted by a large number of pharmacological agents. For example, patients with familial adenomatous polyposis (FAP) have an elevated risk for colorectal cancer and several other types. Ablation of mismatch repair genes in a colon cell line results in accumulation and aberrant activation of mutant KRAS, gain-of-function BRAF, or both. Treatment using ionizing radiation or chemical compounds can induce tumors [35]. Therefore, it is important to understand how we can use natural products or derived compounds to target colon cancer cells specifically without harming normal cells. The purpose of our study was to evaluate if IKK-alpha could be used as a therapeutic target for colorectal cancer cells. We examined its effect on growth, apoptosis, and autophagy in SW480 human colon carcinoma cells using western blotting analysis. The first step was to confirm that we could inhibit IKK-alpha expression by transfection of siRNA oligonucleotides targeting its mRNA sequence. Next, we assessed whether knockdown of IKK-alpha expression would affect cell growth or survival after exposure to H2O2 stressor via colony formation assay and MTT assay respectively. Finally, we tested whether IKK-alpha knockdown affected autophagy by assessing protein levels of LC3B-II through Western blotting. Our data showed that inhibition of IKK-alpha expression resulted in decreased viability and increased apoptosis when exposed to oxidative stress. Moreover, inhibition of IKK-alpha resulted in increased LC3B II protein levels indicating increased autophagic activity [38]. Overall, these findings suggest that down regulation of IKK alpha may be useful for treatment or prevention against colorectal cancer because it protects against oxidative stress induced apoptosis while increasing overall cellular health through up regulation of autophagic activity.\
In-vivo animal experiment for the pharmacological therapeutics of IKK-alpha for colorectal cancer
Studies have shown that inflammation plays a crucial role in initiation and progression of cancer and subsequent colon cancer has been identified as an inflammatory disease. It is well accepted that one of the most important intracellular signalling proteins, IκB kinase (IKK)-α/β, is involved in inflammation and regulation of immune response. Increased expression levels have been reported in colonic epithelial cells from patients with colorectal carcinoma. By up regulating COX-2, Cyclin D1 and Bcl-2 as well as down regulating Myc proto-oncogene expression, various inflammatory cytokines induce growth arrest or apoptosis resistance which may contribute to tumorigenesis [40]. The present study investigates how IKK-α affects proliferation and survival of HT29 cells under different conditions including hypoxia, oxidative stress, and chemotherapeutic drugs doxorubicin (DOX) and cisplatin (CDDP). The results showed that DOX combined with CDDP induced cell death through both apoptotic and necrotic pathways [41]. However, cell death was significantly reduced by pre-treatment with antisense oligodeoxynucleotides against IKK-α. Additionally, overexpression of wild type IKK-α promoted cell survival whereas knockdown resulted in significant decrease in proliferation rate compared to control group. These findings suggest that inhibition of IKK-α could be used as potential therapeutic target for colorectal cancer treatment [42].
Conclusion
To summarize, we propose that targeting IKK-α plays a vital role in preventing colorectal cancer. Therefore, our results suggest that molecules designed to reduce expression or inhibit activity of IKK-α may hold promise as anticancer therapeutics. This is particularly attractive because existing drugs already target IKKβ and therefore could be easily tested for their effects on colon cancer development and progression in mouse models, which would make identifying synergistic pairs possible with greater speed than starting from scratch. Furthermore, these experiments are likely to produce more physiologically relevant results than those using solely genetics or chemical screens. Thus, it seems that there are many reasons to consider IKK-α an attractive therapeutic target for colorectal cancer treatment.
References
- Jack A Prescott, Kathryn Balmanno, Jennifer P Mitchell, et al., Biochem J. 2022, 479: p. 305-325.
- Baker RG, Hayden MS and Ghosh S.Cell Metab. 2011, 13: p. 11-22.
- Li Q, Van Antwerp D, Mercurio F, et al., Science. 1999, 284: p. 321-325.
- Qiutang L, Qingxian L, Hwang JY, et al., Genes Dev. 1999, 13: p. 1322-1328.
- Li X, Massa PE, Hanidu A, et al., J Biol Chem. 2002, 277: p. 45129-45140.
- Sizemore N, Lerner N, Dombrowski N, et al., J Biol Chem. 2002, 277: p. 3863-3869.
- Park JM, Greten FR, Wong A, et al., Immunity. 2005, 23: p. 319-329.
- Ruocco MG, Maeda S, Park JM, et al., J Exp Med. 2005, 201: p. 1677-1687.
- Greten FR, Eckmann L, Greten TF, et al., Cell. 2004, 118: p. 285-296.
- Shibata W, Takaishi S, Muthupalani S, et al., Gastroenterology. 2010, 138: p. 1022-1034.
- Hu Y, Baud V, Delhase M, et al., Science. 1999, 284: p.316-320.
- Plewka D, Plewka A, Miskiewicz A, et al., J Can Res Ther. 2018, 14: p. 516-20.
- Hayden MS, Ghosh S. Signaling to NF‑kappaB. Genes Dev. 2004, 18: p. 2195‑224.
- Karin M, Ben‑Neriah Y. Annu Rev Immunol. 2000, 18: p. 621‑663.
- Luo JL, Kamata H, Karin M. J Clin Invest. 2005, 115: p. 2625‑32.
- Lind DS, Hochwald SN, Malaty J, et al., Surgery. 2001, 130: p. 363‑9.
- Lindholm PF, Bub J, Kaul S, et al., Clin Exp Metastasis. 2000, 18: p. 471‑479.
- Balkwill F, Mantovani A. Lancet. 2001, 357: p. 539‑545.
- Coussens LM, Werb Z. Nature. 2002, 420: p. 860‑878.
- Grivennikov S, Karin E, Terzic J, et al., Cancer Cell. 2009, 15: p. 103‑113.
- Lawrence T, Willoughby DA, Gilroy DW. Nat Rev Immunol. 2002, 2: p. 787‑795.
- Schottenfeld D, Beebe‑Dimmer J. CA Cancer J Clin. 2006, 56: p. 69‑83.
- Huiping Liu, Guoning Li, Bin Zhang, et al., Molecular medicine reports. 2018, 17: p. 5837-5843.
- Wu Y, Yang L, Zhao J, et al., Mol Cancer. 2015, 14: p. 191.
- Chen W, Zheng R, Zhang S, et al., Chin J Cancer Res. 2009, 25: p. 10‑21.
- Nishisho I, Nakamura Y, Miyoshi Y, et al., Science. 1991, 253: p. 665‑669.
- Binefa G, Rodríguez‑Moranta F, Teule A, et al., World J Gastroenterol. 2014, 20: p. 6786‑6808.
- Liu HP, Gao ZH, Cui SX, et al., PLoS One. 2012, 7: p. e33243.
- Chiurillo MA. World J Exp Med. 2015, 5: p. 84‑102.
- Larriba MJ, Ordóñez‑Morán P, Chicote I, et al., PLoS One. 6: p. e23524.
- Carothers AM, Davids JS, Damas BC, et al., Cancer Res. 70: p. 4433‑4442.
- McClellan JL, Davis JM, Steiner JL, et al., Cytokine. 2012, 57: p. 113‑119.
- DeVore RF, Fehrenbacher L, Herbst RS, et al., In Proceedings of American Society of ClinicalOncology. 2000, 19: p. 485a.
- Voortman J, Resende TP, Abou El Hassan MA, et al., Mol Cancer Ther. 2007, 6(7): p. 2103–2112.
- Davies AM, Lara PN, Mack PC, et al., Clinical Cancer Research, 2007, 13: p. s4647-4651.
- Lynch TJ, Fenton D, Hirsh V, et al., J. Thorac. Oncol. 2009, 4(8): p. 1002–1009.
- Das KC, White CW. J Biol Chem. 1997, 272 (23): p. 14914-14920.
- Baker AF, Hanke NT, Sands BJ, et al., J Exp Clin Cancer Res. 2014, 33(1): p. 111.
- Dermawan K. Gurova J Pink JKT, Dowlati A, et al., Mol Cancer Ther. 2014, (9): p. 2203–2214.
- Davies AM, Ho C, Metzger AS, et al., J Thorac Oncol. 2007, 2(12): p. 1112–1116.
- Tomita M, Wright J, Kellogg R, et al., Lung Cancer. 2005, 49: p. S329.
- Denlinger CE, Rundall BK, Keller MD, et al., Ann Thorac Surg. 2004, 78: p. 1207–1214.
- Arnold SM, Chansky K, Leggas M, et al., Invest New Drugs. 2017, p. 1-8
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref