Review Article - Der Pharma Chemica ( 2024) Volume 16, Issue 1
In-Situ Gel Systems for Ocular Therapeutics: Unveiling the Impact of Polymer Selection
Aakanksha Sinha1*, Vishal Das1, Ramakant Yadav2 and S. J. Daharwal12Department of Pharmacy, Gurunanak Institute of Research and Development, Maharashtra, India
Aakanksha Sinha, Department of Pharmacy, Pt. Ravishankar Shukla University, Raipur, Chhattisgarh, India, Email: aakanksha01121@gmail.com
Received: 31-Jan-2024, Manuscript No. DPC-23-126414; Editor assigned: 05-Feb-2024, Pre QC No. DPC-23-126414 (PQ); Reviewed: 20-Feb-2024, QC No. DPC-23-126414; Revised: 29-Jan-2024, Manuscript No. DPC-23-126414 (R); Published: 26-Feb-2024, DOI: 10.4172/0975-413X.16.1.224-231
Abstract
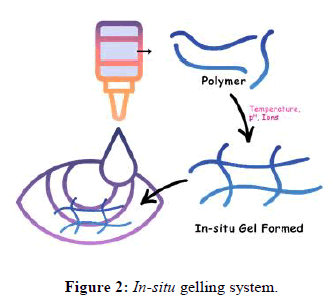
A major problem in ocular therapeutics is the attainment of optimal drug concentration at the site of action, which is mainly due to precorneal loss resulting in only a small fraction of the drug being ocularly absorbed. Ensuring the use of in-situ gel-forming technologies, the effective dose can be changed by altering the medication's retention duration in the eye. The "in situ gel" system has become one of the top cutting-edge drug delivery systems; its special "sol to gel" transition feature helps with the controlled and continuous release of medications. An in-situ gelling system is a formulation that, before it enters the body, stays in the liquid form but that, when subjected to specific physiological circumstances, transforms into gel form. Various polymers are subjected to in situ gel formation and could be employed for a variety of drug administration routes. In today's world, the in-situ gelling system has a variety of uses and benefits. This paper focuses on an overview of in situ gels, their mechanisms, the various polymers utilized and their applications in situ gel, novel drug delivery system, polymers.
Keywords
In-situ gel; Ocular drug delivery system; Polymers
Introduction
The primary aim of any drug delivery system is to modify the pharmacokinetic parameters and the tissue distribution of the drug in a useful way. The development of controlled and sustained energy has received a lot of attention over the last 60 years release drug delivery systems. Various natural and synthetic polymers are used for development of in situ gel drug delivery systems. Out of all the concerns for pharmaceutical scientists has continued to be ocular medication delivery. Eye's distinctive structure prevents medication molecules from entering the required spot of action. Anterior and posterior segments can be used to broadly classify drug distribution to the eye. Conventional methods for treating vision threatening ocular illnesses, such as eye drops, suspensions and ointments, can't be considered as optimal. However, eye drops make for greater than 90% of the commercially available ophthalmic formulations [1-3]. Additionally, the human cornea's endothelium, substantia propria and epithelium all prevent drug molecules from entering the eye. The above mentioned factors, less than 5% of the medication that is delivered enters the eye. One of the appropriate ways to increase the contact time and bioavailability is achieved by use of mucoadhesive polymers. In situ gelling system will cover all the limitations of conventional dosage form and as a drop which is easily dropped in to the eye. This upon exposure to physiological conditions will shift to the gel phase. Various substances include sodium alginate, poloxamer, carbomers, carbopol or its derivatives changed from sol to gel as pH changes. As therefore, this kind of formulations has advantages over both solutions and gels. They may also increase drug retention time while also improving formulation accuracy and administration simplicity. In situ gelling systems consist of polymers which in the cul-de-sac display sol-to-gel phase transitions as a result of physicochemical changes parameters such as temperature, pH and ionic strength in the environment. Although these may reduce the frequency of topical administration, in situ gelling technology have emerged as promising ocular drug delivery platforms. Their benefits come from a solution to gel phase shift that causes prolonged ocular surface residence. This may improve drug absorption in the eye, improving therapeutic results. Additionally, decreasing the pre-corneal clearance of the gel after ocular administration eliminates absorption into systemic circulation and may thus minimize negative effects. Due to its specific benefits, the study of ophthalmic in situ gels is one of the most popular areas in the administration of ocular drugs. Researchers usually combine two or more environmentally sensitive polymers with synergistic action to decrease the overall concentration of each polymer. In situ gels can be used in conjunction with nanoparticle drug delivery methods such polymer micelle nanosuspensions, according to current literature. The benefits of in situ gels and nanoparticles can be combined in this manner. Studies using these mixtures have shown improved ocular bioavailability of water-insoluble medications, as well as precise dosing, controlled release and few adverse effects of the delivered medications. Biodegradable polymers including poly-caprolactone, polyD-lactic acid, in-situ gelling agents include gellan gum, pectin, chitosan, alginic acid, xyloglucan, poly-DL-lactide-co-glycolide and poly-caprolactone gel system [4,5]. In the ocular delivery system organic polymers that are alginic acid, inulin and xyloglucan, inulin is widely used. In the local system availability of different ophthalmic to treat intraocular intolerance in glaucoma, chemicals such as independent medicines, anti-inflammatory agents and antibacterial agents are employed. The standard delivery system is often found to be unavailable and therapeutic response due to excessive fluid retention and energy leading to the rapid elimination of the drug in the eye and therefore, overcoming the problem of ophthalmic bioavailability an in-situ gel was used. Increasing the viscosity with substances like carboxymethylcellulose, hydroxypropyl methylcellulose, carbomers and poly vinyl alcohol improve bioavailability is used to improve the viscosity of the composition to extend the earlier stay and increase availability, which is easier to do. Entry enhancement as a protective, deceptive agent, surfactants used to improve corneal drug penetration.
Literature Review
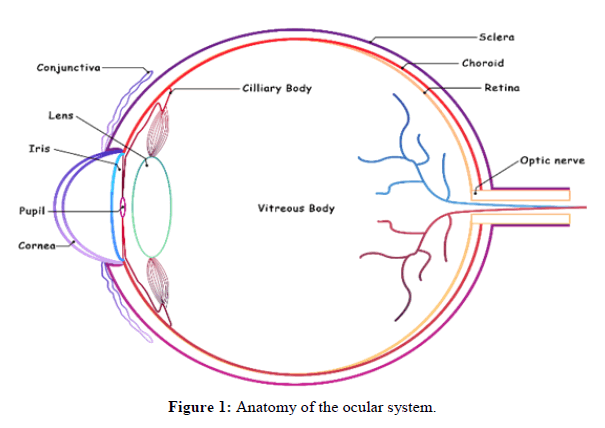
Anatomy of the ocular system
The human eye's anterior and posterior segments are divided into two distinct segments. The conjunctiva, pupil, anterior chamber, lens, cornea iris, culinary body, aqueous fluid and trabecular meshwork make up the anterior segment. The cornea's outer membrane consists of five levels epithelium, bowman's layer, stroma, descemet's membrane and endothelium. The transparent both posterior and anterior chambers of the eye are filled with liquid is known as aqueous humour. Its primary job is to give nutrition, eliminate waste from non-vascular tissues and maintain the cornea's convex shape by controlling intraocular pressure (Figure 1) [6-8].
In the iris a little circular curtain positioned in front of the lens but back of the cornea. It is a variable size diaphragm whose job is to regulate the brightness entering the eye by adjusting the pupil size. The smooth muscular ciliary muscle, located in the middle of the eye, controls visual field. The lens is a bi-convex transparent construction with a small transparent lens cover. A mucous membrane called the conjunctiva covers the inside of the eyelid and the corner of the eye, the sclera and the limbus. It protects the eyes by massaging them and eliminating mucus membranes. The sclera is the translucent, elastic and white portion of the eye made up of collagen fibers. The sclera serves as a protective outer layer while also controlling intraocular pressure and connecting the extraocular muscles. The second layer of the eye, the choroid, situated between the retina and sclera. An extremely thin coating of veins with dark brown veins that contains a pigment that absorbs excess light and thus prevents fuzzy vision. The retina is a multilayered and intricate structure made up of vascular, glial and neuronal cells as well as nerve fibers. The process of vision generation begins in the retina, where light is turned into signals by specialized cells known as photoreceptor cells, which are then interpreted inside the brain to create vision [9-11].
In situ gelling system
In the early 1980’s, the revolutionary notion of in situ gel manufacturing was initially introduced. Ocular in-situ gelling systems are ocular medication delivery devices that can transition between phases minor variations in certain parameters such as pH, temperature and ionic strength. In this medication delivery device, the solution is injected with gelation in situ before being delivered to the body, generating a gel in the cul-de-sac of the eye. A fluid or suspension in the form of a gel that has certain viscoelastic and bio adhesive properties. The in-situ gel's residence time is increased as a result and the medication is delivered continuously resulting in increased bioavailability, lower systemic absorption and a less frequent dosage regimen, all of which lead to greater patient compliance. Pharmaceutical companies, with the support of their formulation development teams, have made great progress in this polymer technology, which has the remarkable ability to convert from a free-flowing transparent liquid to a viscous gel in an instant [12-15]. In situ gels can be made from both natural and synthetic polymers. Poloxamer 407 (P407) and Poloxamer 188 (P188), for example, are polymers that are frequently utilized in ocular medication formulations due to their good water solubility, solution clarity and shear thinning behavior and safety to ocular tissues (Figure 2 and Table 1).
| Stimuli mechanism | Mechanism | Examples |
|---|---|---|
| PH change | Sol to gel transition when pH rises from 4.2-7.4. At higher pH polymer forms hydrogen bond with mucin which leads to formation of hydrogel network. | Pseodolatexes carbomer (acrylic acid) cellulose acetate, phthalate latex |
| Ionic interactions | Formulation undergoes liquid gel transition under influence of an increase in ionic strength gel formation takes place because of complexation with polyvalent cations (like Ca+) in lacrimal fluid. | Chitosan, gellan gum/gelrite alginate |
| Temperature | Formulation is liquid at room temperature (20°C-25°C) which undergoes gelation in contact with body fluid (35°C-37°C). Temp increases degradation of polymer chains which leads to formation of hydrophobic domains and transition of an aqueous liquid to hydrogel network. | Poloxamer/phloronics xyloglucan cellulose derivative |
Table 1: Mechanism of in situ gelling system.
Importance of in situ gelling system
• Assists in the medication is released in a regulated and sustained manner thanks to the 'sol gel transition.'
• It is desirable to use a liquid dosage form that can maintain medication release and stay in contact with the cornea of the eye for a longer period of time.
• It aids in the reduction of drug administration frequency in the body.
• Only a small amount of the drug is needed and there will be no drug buildup or adverse effects.
• The drug's bioavailability will be increased.
• Because of the gel formation, the medicine will have a longer residence period.
• The in-situ gel technology reduces drug wastage.
• Drugs drained through the nasolacrimal duct have a lower systemic absorption rate, which might cause unwanted side effects.
Advantages of in situ gel system
• Less obscured eyesight than ointment.
• Ease of medication administration.
• Its manufacturing is less complex, resulting in lower investment and manufacturing costs.
• It can be given to patients who are unconscious.
• Increased patient satisfaction and compliance.
• Reducing the number of doses and drug toxicity.
• Natural polymers naturally promote cellular functions by being biocompatible, biodegradable and composed of physiologically recognizable
moieties.
• It also is engineered to exhibit bio adhesiveness to facilitate drug targeting, especially through mucus membranes, for non-invasive drug administration.
• In situ gels offer an important "stealth" characteristic in vivo, owing to their hydrophilicity, which increases the in vivo circulation time of the delivery device by evading degradation.
Disadvantages of in situ gel system
• It necessitates a large amount of fluids.
• The drug's sol form is more sensitive to deterioration.
• Chemical deterioration could cause stability issues.
• Eating and drinking may be restricted for several hours after the medication is implanted.
• Drug loading into hydrogels may be limited in terms of amount and uniformity, especially for hydrophobic drug.
• Only medications with a low dose requirement can be administered.
• Lower mechanical strength can lead to early failure.
• The hydrogel dissolves or flows away from a specific local spot.
Approaches
There are 4 mechanisms for triggering the in-situ gelling formation of biomaterials. These include: In situ gel formation due to physiological stimuli
• Temperature triggered in situ gel systems
• pH triggered in situ gel
In situ gel formation due to ion activated system
In situ gel formation due to physical mechanism
• Swelling
• Diffusion
In situ gel formation due to chemical reactions
• Ionic cross-linking
• Enzymatically cross-linking
• Photo-polymerization
Discussion
Mechanism of in situ gels
The mechanism of in situ gels is based on following mechanisms:
Swelling: In this method of in-situ gel formation the material absorbs water from its surroundings and expands to fill the necessary space. Glycerol monooleate, for example, is a polar lipid that expands in water and forms lyotropic liquid crystalline phase structures. It has some bio adhesive qualities and is enzymatically destroyed in vivo.
Diffusion: In this procedure, the solvent from the polymer solution diffuses into the surrounding tissue which the polymer matrix precipitates or solidifies as a result. The solvent N-Methyl Pyrrolidone (NMP) has been proven to have effect in such a system.
Based on the mechanics of chemical reactions
Precipitation of inorganic solids from supersaturated ionic solutions, enzymatic activities and photo-initiated processes are all examples of chemical reactions that result in in situ gelation (Table 2) [16-19].
| Diffusion controlled | Swelling controlled | Chemically controlled |
|---|---|---|
| (Drug diffusion from the non-degraded polymer) | (Enhanced drug diffusion due to the polymer) | (Drug release due to polymer degradation and erosion) |
Table 2: Drug Release from in situ Gels.
Temperature triggered in-situ gel systems
The in situ thermoreversible gel is a technology that responds to temperature changes and converts fluid into gel form at a defined temperature range. The use of a polymer that transforms from solution to gel at the temperature of the eye can provide long-term medication delivery. The gel can be injected into the eye in liquid form and is produced at a precorneal temperature of 35 degrees celsius. A gel-sol transition must occur at the precorneal temperature for this type of gel and it must have a gelation temperature higher than room temperature. Therefore, it is not advised to store the formulation in the refrigerator before application as the cool temperature may cause eye pain.
Polymers used in temperature triggered in-situ gel system
Poloxamers (Pluronic): Poly (ethylene oxide)-b-poly (propylene oxide)-b-poly (ethylene oxide)-b-poly (ethylene oxide)-b-poly (ethylene oxide)-bpoly (ethylene oxide)-b-poly (ethylene oxide)-b-poly (ethylene oxide)-b-poly (ethylene oxide)-b-poly (ethylene oxide)-b-poly (PEO-PPOPEO) ethylene oxide domains that are hydrophilic and propylene oxide domains that are hydrophobic At concentrations greater than 15% (w/w), the copolymer triple block PEO-PPO-PEO (Poloxamers or pluronics) gels temperature of the human body.
A solution of 0.1 percent w/w alginate or 0.3 percent w/w carbopol and 14 percent w/v poloxamer was found to be free flowing at pH 4.0 and 25°C. These mixtures gelled with a significant increase in gel strength under physiological conditions. Using polymer combinations, the improved ocular bioavailability of pilocarpine hydrochloride was proven investigations done in vivo and in vitro.
Wei and his colleagues were employed as a model; researchers developed and evaluated two heat sensitive in situ gels made with poloxamer 407 and methylcellulose and employed betaxol, a beta-adrenergic receptor inhibitor allowed to treat chronic open-angle glaucoma or ocular hypertension. Consequently, the researchers were interested in learning how drug release affected the kind of gel and the temperature at which it gelled. The effectiveness of the in-situ gel medicine was also examined. The delivery method performed similarly to the industrial resin suspension in vivo. There were experiments done specifically in vitro. To measure the distribution of the medication, in vivo pharmacokinetic studies were carried out to evaluate betaxol release. The FDA has approved betaxol (Betoptic S® China Pioneer Pharma Holdings Limited, Shanghai) eye drops. These suspension eye drops are commercially available and use ion exchange (IR) resins to facilitate drug release. They were tested and compared to in ocular tissue in situ gels. According to in vivo pharmacokinetic investigations, the in-situ gels performed better than the ex-situ gels at increasing drug concentration in the cornea.
Choi et al., described a magnetic stirring bar approach for rectal usage that utilized an in-situ cellulose derivatives and poloxamers based gelling formulation. Then, employing this technology, several thermosensitive ophthalmic delivery devices were created. A vial with a magnetic bar and a digital thermometer is filled with the mixture and the vial is then immersed in water. The combination is then heated continuously at a rate of 0.5 to 20 degrees celsius per minute, depending on the needs. Lastly, the gelation temperature is the temperature that the thermometer reads when the magnetic bar stops stirring as a result of formulation gelation.
Xyloglucan: It’s a natural polymer having a backbone of b-(1-4)-glucose residues and a-(1-6)-xylose side chains that are partially replaced by b-(1-2)-galactoxylose. Heptasaccharide, octasaccharide and nonasaccharide are three units of xyloglucan oligomers with different numbers of galactose side chains. It has a very weak phase transition property. In the presence of b-galactosidase, however, partial polymer breakdown causes thermally induced in situ gelation. This temperature sensitivity appears only when the galactose removal ratio hits 35%.
Mannuci et al., revealed that tamarind seed polysaccharide may crystallize and that following crystallization; it had a fernlike structure, making it similar to tear secretions. The tamarind seed solution potential to stay on the ocular surface for an extended amount of time and is similar to endogenous mucin. As a result, it is an excellent choice for treating dry eyes. Recent research it was discovered that tamarind seed solution outperformed hyaluronic acid because of its increased viscosity, which allows for longer retention.
Miyazaki et al., The effectiveness of xyloglucan and PF-127 sols as long-acting drug delivery systems for pilocarpine hydrochloride was examined in rabbits. Pilocarpine was released in vitro over a period of six hours from gels created by heating xyloglucansols (1.0, 1.5 and 2.0 percent, w/w) to 34°C. All gels exhibited sustained pilocarpine release and as the xyloglucan content grew, so did the length of the miotic reaction. In comparison to a 25 percent (w/w) PF-127 gel, a 1.5 percent (w/w) xyloglucan gel produced a sustained pilocarpine release that increased the miotic response to a similar extent.
Burgalassi et al., found that XG made from tamarind seed forms a thermoresponsive gel in water under specified circumstances. Despite having a low viscosity, the XG-containing formulation produced high levels of timolol in the ocular tissues and little systemic absorption. According to Shahiwala, the XG vehicle performed comparable to the reference in situ gelling formulation (Timoptic XE).
Chitosan: Chitosan is a sugar derived mostly from the shells of shellfish, shrimp, lobsters and crabs. It's most commonly used as a dietary supplement. It's manufactured by soaking chitin coated shells of the crustaceans listed above in an alkaline solution for example, sodium hydroxide. It's a linear polysaccharide made up of deacetylated and acetylated units that are randomly dispersed-(140)-linked D-glucosamine and N-acetyl- Dglucosamine. Chitosan is frequently employed in the biomedical area because of its beneficial properties such as mucoadhesiveness, biocompatibility, low cytotoxicity and biodegradability [20].
Gupta et al. created an in-situ gel for the ocular release of the antiglaucoma drug timolol maleate using chitosan and poloxamer. Chitosan, a pH-sensitive polymer, was used to increase permeability while Pluronic F-127, a thermosensitive polymer, was used as a gelling agent. Chitosan increased the transcorneal permeability of timolol. It had bioadhesive qualities, was viscous and had the capacity to gel at ocular pH 7.4. When the in vitro transcorneal permeability test was performed on goat cornea after four hours, the in-situ gelling approach demonstrated improved penetration contrasted with eye drops. This was the case because chitosan could increase transmucosal permeability.
de Campos et al., in 2001, demonstrated that cyclosporin A loaded chitosan nanoparticles formulated by ionic gelation technique enhanced the therapeutic level of drug when instilled in ocular tissues as compared to aqueous solution of cyclosorin A and showed faster release of drug within the first hour, then a slow gradual release (Table 3).
| Model drugs | Polymers | Major finding |
|---|---|---|
| Brinzolamide | Poloxamer F127 and carbopol 934P | Over the course of eight hours, a sol-gel at 33.2 1.1°C controlled the release of the medication. |
| Ofloxacin | Pluronic (PF-127 and PF-68) and sodium alginate | Extended its stay and increased its ocular availability. |
| Ketorolac tromethamine | Pluronic F-127 HPMC K4M | Improved its ocular availability and prolonged its residence time. |
| Lomefloxacin | Pluronic F127, Pluronic F68 and sodium alginate | Revealed an 8-hour continuous release profile. |
| Methazolamide | Poloxamer 407 and poloxamer P188 | Compared to ocular drops, had a superior capacity to keep the medication. |
| Dorzolamide hydrochloride | Poloxamer 407 and Poloxamer 188 | Compared to either the medication solution or the market product, a better pharmacological effect with a quicker beginning of action and a longer-lasting effect. |
| Diclofenac sodium | Pluronic F127 | Diclofenac sodium's bioavailability in aqueous humour was markedly improved. |
| Sparfloxacin | Pluronic (PF 127 and PF 68) | Both in vivo and in vitro tests revealed promising antibacterial efficacy. |
| Fluconazole | Poloxamer/tween/carbopol | Comparing the in vivo ophthalmic absorption to the standard eye drop. |
Table 3: Some examples of thermo-sensitive in situ gelling system.
pH triggered in situ gelling systems
pH-sensitive delivery systems that gel in situ are another an essential category of sol-gel formulations particularly for ocular delivery. The external pH environment is the second type of stimuli responsive method. Polyelectrolytes are the most common of these polymers with repeating units of either basic or acidic groups. It shows swelling properties with increasing ambient pH in weak acidic group polymers (polyacids) and vice versa in weak basic group polymers (polybases). At a lower pH (pH 4.4), the formulation is a standard solution, but at a higher pH (pH 7.4), tear fluid's pH, it gels. Carbopol, carbomer, or variants are the most common pH-sensitive anionic polymers.
Polymers used in pH triggered in situ gel systems
Carbopol (Polyacrylic acid): Carbopol is a kind of carbopol (Polyacrylic acid) carbopol is a gel-forming Polyacrylic Acid (PAA) polymer as the pH rises over cheval cheval (4.0 to 7.4). At acidic pH, carbopol remains in solution, while at alkaline pH, it transforms into a low viscosity gel. When HPMC is combined with carbopol, the viscosity of the carbopol solution is increased while the acidity of the solution is.
Kouchak et al., pH-triggered in situ gel delivery technique for the ophthalmic administration of the ocular hypertension drug Dorzolamide (DRZ) was created by different percentages of carbopol and HPMC were used, but it turned out that 0.1 percent was the best concentration for both polymers since it behaved in both cases as a pseudoplastic fluid. In vivo investigations and experiments revealed that this carrier was more effective at sustaining DRZ than the conventional DRZ solution. Additionally, the drug's precorneal residence time was prolonged due to its high in situ viscosity and mucoadhesive property, which boosted bioavailability, decreased administration frequency and decreased systemic side effects. This formulation may therefore be a good substitute for DRZ eye drops.
According to Oechsner, et al., Polyvinylpyrrolidone (PVP) was mixed with the polymer PAA (0.1-0.2 percent, w/w) at a concentration of 6% (w/w). Once PVP was added, the mixture's apparent viscosity was greatly lowered. This is crucial for minimizing the discomfort caused to the eyes by systems using high viscosity gels comprised completely of PAA. The combination of the two polymers, PAA and PVP, may be helpful for the treatment of dry eyes because the formulation had a low viscosity and a high mucoadhesion index compared to the monopolymer PAA preparation.
Nanjwade et al., developed and tested an ocular delivery system for ketorolac tromethamine based on the pH-triggered in situ gelation idea, using polyacrylic acid (Carbopol® 934) as the gelling agent and HPMC (Methocel K4M) as the viscosity enhancer. It was discovered that the formulation was stable, non-irritating, therapeutically efficacious and capable of delivering an 8-hour sustained release of the medication in vitro. According to the research, the developed because of its capacity to increase bioavailability through its formulation, it is a feasible alternative to traditional eye drops prolonged precorneal residence period and the ability to produce long-term drug release (Table 4).
| Model drugs | Polymers | Major finding |
|---|---|---|
| Baicalin | Carbopol 974P with HPMC E4M | When compared to commercial baicalin eye drops, this medication has better stability, ocular bioavailability and sustained drug release. |
| Ciprofloxacin | Calcium alginate with HPMC K4M and E50LV | Additional advantages of prolonged medication release. |
| Norfloxacin | Carbopol 934P | Antibacterial action, adequate mucoadhesion and no eye irritation. |
| Timolol Maleate | Carbopol and chitosan | Exhibited the controlled release across 24 hour periods. |
| Brimonidine | Carbopol 974 P and HPMC E4M | Brimonidine tartrate has improved effectiveness and decreased systemic absorption. |
| Gatifloxacin | Carbopol 940 combined with HPMC and HPMC K15M | Provided eight hours of continuous medication release. |
| Moxifloxacin | Carbopol/HPMC | exhibited enhanced ocular bioavailability and precorneal residence duration |
Table 4: Some examples of pH-triggered in situ gelling system.
Ion activated in situ gel systems In this procedure, a change in ionic strength causes the injected solution to gel. Ion-sensitive polysaccharides may produce in situ gel on the ocular surface by cross-linking with cations in tear fluid. Anionic polysaccharides gel when cations like Na+, Mg++ and Ca++ are present in the tear fluid. The produced in situ gel prolongs precorneal contact time, resulting in increased bioavailability. Gelrite gels while it gets delivered because calcium ions are present. The formation of double helical junction zones, which are caused by cation complexation and hydrogen bonding with water, is the first step in the gelation process. Next, double helical segments accumulate to form three-dimensional networks.
In situ gel-forming eye drops based on estradiol activated by ions were developed to help older people avoid cataracts. In order to promote medication solubility, mannitol was added to control tonicity, polysorbate-80 was used as an ion-activated gelling polymer, gellan gum was used as an ion-activated gelling polymer and preservatives potassium sorbate and disodium Edetate Dihydrate (EDTA) were also added. The solution eye drops gelled when combined with artificial tear fluid and viscoelastic experiments supported gel formation. 80 percent of the gel's medication was released in significant amounts in just 8 hours. The formulations exhibited viscoelastic behavior for 6 months under rapid and long-term storage conditions and were transparent, isotonic and stable. The results suggest that the formulation based on estradiol may be useful in preventing and delaying cataracts as a result.
Carlfors et al., investigated the relationship between mucoadhesive and the rheological qualities of gellan gum-containing gels. Benzalkonium chloride (0%-0.02%) and glycerol (0%-4%) were heated for 20 minutes at 90°C to make different amounts of gellan gum (0.4%-1.2%) solutions. Glycerol and benzalkonium chloride were used to achieve various osmolalities. The flexibility of the gel increases as the concentration of electrolytes rises. The flexibility of the gels was not affected by the concentration of gellan gum in the electrolyte solution. By lowering the formulation osmolality, the gel's retention time was raised to 20 hours.
Zhu et al., produced ion-activated ketotifen ocular formulations using the natural polysaccharide deacetylase gellan gum. The research revealed that the residence time of the formulation might be increased by deacetylase gellan gum. The in-situ gels demonstrated characteristic sustained and extended drug effects behavior as compared to conventional eye drops at the same dose.
Sodium alginate
Sodium alginate is a brown algae-derived gum. It's a salt of alginic acid D-Mannuronic acid and L-Glucouronic acid residues are linked together by 1,4-glycosidic bonds to form a linear block polysaccharide connection. Because of the carboxylic group, it has a good mucoadhesive characteristic. It decomposes naturally and is non-toxic. Its molecular weight ranges from 20 kDa to 600 kDa. D-mannuronic acid and -L-glucuronic acid residues are joined by 1,4-glycosidic linkages to form the linear block copolymer polysaccharide known as algaenic acid. The percentage of each block and how they are arranged along the molecule vary according on the algal source. Sequential glucuronic residues in the -L-glucuronic acid blocks of the alginate chain cooperate to create gels when di and trivalent metal ions are introduced to diluted aqueous solutions of alginates. Cohen et al., the effect of guluronic acid content on the sol-gel transition of alginate dispersions was examined and an alginic acid pilocarpine formulation was created for drug delivery to rabbit eyes. Alginates (0.5 percent w/w) quickly gel in the simulated tear fluid and have a high guluronic acid concentration (N65 percent). It has been demonstrated that pilocarpine works in vivo. In treated rabbit eyes, the formulation, which contained 1% alginic acid (and 69% guluronic acid), significantly lowered intraocular pressure for around 10 hours. Pilocarpine solution had a 3-hour reduction in intraocular pressure. A pilocarpine-loaded alginic acid formulation with a low guluronic acid content (39%) was also found to be comparable to pilocarpine solution by the in vivo results. Alginic acid formulations have also been developed for ophthalmic administration of beta-adrenergic blockers and ciprofloxacin for the treatment of glaucoma and ocular infections. According to these studies, alginic acid has the potential to be a medicine carrier that lowers the frequency of instillations while increasing patient tolerability.
Sechoy et al., compared alginic acid and Hydroxyethyl Cellulose (HEC) as in situ gelling methods for prolonged administration of carteolol. Alginic acid demonstrated better adhesion properties with a mucin-coated ocular surface than HEC did, despite the fact that the viscosity of both alginic acid and HEC-based forms was almost comparable. It's probable that an ionic interaction between carteolol and alginic acid is the cause of carteolol's slower diffusion. But in the case of formulations including alginic acid, higher levels of carteolol were discovered in the aqueous humour. The formulation's AUC08 hr increased by about 50% after alginic acid was added. Neither formulation's carteolol concentration in the iris or ciliary body changed after 15 days of therapy. Carteolol-alginic acid eye drops had excellent ocular tolerability, causing no discomfort or histological changes. The peak plasma concentration of formulations with alginic acid was lower than that of a simple carteolol solution. The in-situ gelling devices based on alginic acid can reduce the frequency of carteolol doses from twice to once per day. Motwani et al., to prolong the release of the drug at the ocular surface, created chitosan-sodium alginate nanoparticles loaded with gatifloxacin by ionic gelation or modified coacervation technique. They observed that the drug was released in a sustained manner by non-fickian diffusion (Table 5).
| Model drugs | Polymers | Major finding |
|---|---|---|
| Gatifloxacin | Alginate with HPMC | Compared to standard ophthalmic solutions, a better ocular bioavailability and longer residence duration in aqueous humour. |
| Fluconazole | HPBCD complexed gellan gum and κ-carrageenan | Showed good bioadhesive qualities and demonstrated efficient control of fluconazole release. |
| Acetazolamide | Gellan gum with xanthan gum, HPMC or carbopol. | Superior therapeutic effectiveness and a longer-lasting effect in lowering intraocular pressure when compared to commercially available eye drops and oral tablets. |
| Terbinafine hydrochloride | Gellan gum | Improved bioavailability, significantly greater Cmax, postponed tmax and longer mean residence time. |
| Antisense oligodeoxynucleotide | Gellan gum and carrageenan | Least stromal edema and hypercellularity and the highest reduction in wound size |
Table 5: A few illustrations of in situ gelling systems that are ion-activated.
| Name of the product | Polymer | The type of in situ gelling system | Company |
|---|---|---|---|
| Timoptic-XE® (Timolol maleate ophthalmic gel forming solution) | Gellan gum | Ion-induced | Merck pharmaceuticals, USA |
| Pilopine HS® (pilocarpine hydrochloride ophthalmic gel) | Carbopol 940 | pH-triggered | Alcon laboratories, inc. USA |
| Akten® (Lidocaine hydrochloride) | HPMC | Temperature-triggered | Akorn Inc., lake forest, IL |
| AzaSite (azithromycin ophthalmic solution) | Poloxamer 407 | Temperature-triggered | InSite Vision |
| Timoptol-LA (Timolol maleate) | Gellan gum | Ion-activated | Laboratories Merck Sharp and Dohme |
| Virgan (Ganciclovir) | Carbopol® 974 | pH-triggered | Laboratoires THEA-France |
Table 6: List of marketed formulation of in-situ gel.
Evaluation
Evaluation parameters: The following parameters can be examined using in situ gel.
Visual appearance and clarity: Ocular in-situ gelling systems are done to check the presence of any small, particulate substances by utilizing fluorescent light against a black and white background.
pH measurement: pH affects both solubility as well as stability of drug in ophthalmic formulations. In order for the patient to not become irritated, it should be such that the formulation will remain stable at that pH.
Drug content: To achieve dosage uniformity, the active component must be distributed uniformly. The drug content was obtained by diluting 1 ml of the formulation to 100 ml of ATF solution pH 7.4. A 1 ml aliquot was collected and diluted with STF water to 10 ml.
Gelling capacity: This evaluation is necessary to know the time taken by the formulation to phase transit from sol to gel. The gelling capacity of the in-situ formulations is usually determined by making use of simulated tear fluid or STF. 0.5 ml-1 ml of a formulation is placed in the 2.0 ml-3.0 ml of STF and the time taken by the dropped formulation to transform to a gel is noted.
Rheological studies: The Brookfield viscometer is primarily used to measure the viscosity of in situ eye gels. By gradually increasing angular velocity from 0.5 to 100 rpm, viscosity is assessed both before and after gelation.
In vitro release studies: Using a made specifically dissolves testing apparatus and a cellophane membrane, the in vitro release of medicine from the formulations was examined. Freshly manufactured artificial tear fluid (7.4 pH) was used as the dissolving medium in this study. A specially constructed glass cylinder that was 5 cm in diameter and open at both ends was submerged overnight in the dissolution liquid and one end of the cylinder was linked to a cellophane membrane. 1 ml of the formulation was carefully pipetted into this assemblage. At a temperature of 37°C, the cylinder was suspended in 50 mL of dissolving liquid with the membrane just contacting the receptor medium. The dissolving media was stirred by a magnetic stirrer at a speed of 50 rpm. Aliquots of 1 ml volume were taken out at regular intervals and replaced with an equal volume of receptor media.
Isotonicity: To prevent any tissue damage or eye irritation, it's crucial for ophthalmic formulations to retain their isotonicity. This phrase alludes to the osmotic pressure that salts in aqueous solution exert. Osmotic pressure in ophthalmic formulations must be between 290 and 310 mol/kg. Osmometers are used to measure tonicity.
Accelerated stability study: To determine the formulation's physical stability under accelerated storage circumstances, a stability study for the in-situ formulation is conducted in accordance with ICH criteria. The formulation is exposed to high humidity and temperature conditions of 25°C/60°RH, 30°C/65°RH and 40°C/755% RH. Samples are taken out after 0, 30, 60 and 90 days and their active medication content is then assessed medication content for evaluating medication content 2 to 3 ml of the formulation is first dissolved in 100 ml of phosphate buffer and then the solution is examined in a UV spectrophotometer.
Antimicrobial activity: Antimicrobial research was performed to determine the biological activity of sol-gel-system antibodies. This is done using the agar diffusion medium using the 'cup techniques'. The microbial growth rate is measured by a combination of antibiotics and compared with those produced with a known concentration of standard antimicrobial formulations and a microbial assay serial dilution method is used.
Conclusion
Ophthalmic delivery systems that gel in place can better treat diseases of the anterior segment of the eye and may be used to create a number of APIs. In the rapidly developing field of ocular medication delivery, most researchers are taking on challenges to address a variety of issues related to this delivery. Continuous technological advancements and steady progress in our understanding of the laws and mechanisms governing the uptake and elimination of drugs into the eye have undoubtedly improved the efficacy of ophthalmic delivery systems. A successful controlled release product's main requirement is to improve patient compliance using in-situ gels. In situ gelling systems, which have grown in popularity recently, are prospective ocular delivery systems since they can get beyond the drawbacks of conventional ocular dosage forms. Researchers in ophthalmology are especially interested in in situ gelling medicine delivery systems. They improve patient compliance and are easy to use. The key advantages of these systems include the capacity to deliver exact and repeatable dosages of drugs, increased pre corneal contact time, delayed drug release, drug distribution to deeper tissues and decreased administration frequency. To further improve and increase the efficiency of drug delivery, these systems can be supplemented by drug-loaded nanoparticles, liposomes or other colloidal drug carriers. Future formulations of in-situ gel that include biodegradable and water soluble polymers may be more palatable and efficient drug delivery techniques. Additionally, in situ gels are simple to commercialize, which is advantageous from an industrial standpoint.
Competing Interests
Authors report no conflict of interest concerning this review article.
References
- Singh M, Dev D, Prasad DN. J Drug Deliv Ther. 2021; 11(6): p. 195-205.
- Wu Y, Liu Y, Li X, et al. Asian J Pharm Sci. 2019; 14(1): p. 1-5.
[Crossref] [Google Scholar] [PubMed]
- Chhetri P, Chakraborty P, Das D, et al. J Drug Deliv Ther. 2021; 11(3): p. 98-103.
- Perminaite K, Marksa M, Stanciauskaite M, et al. Molecules. 2021; 26(12): p. 355-357.
[Crossref] [Google Scholar] [PubMed]
- Agrawal M, Saraf S, Dubey SK, et al. J Control Release. 2020; 327: p. 235-265.
[Crossref] [Google Scholar] [PubMed]
- Agrawal AK, Das M, Jain S. Expert Opin Drug Deliv. 2012; 9(4): p. 383-402.
[Crossref] [Google Scholar] [PubMed]
- Cassano R, Di Gioia ML, Trombino S. Gels. 2021; 7(3): p. 130-144.
[Crossref] [Google Scholar] [PubMed]
- Pandey M, Choudhury H, binti Abd Aziz A, et al. Polymers. 2021; 13(8): p. 1340.
[Crossref] [Google Scholar] [PubMed]
- Destruel PL, Zeng N, Maury M, et al. Drug Discov Today. 2017; 22(4): p. 638-651.
[Crossref] [Google Scholar] [PubMed]
- Chowhan A, Giri TK. Int J Biol Macromol. 2020; 150: p. 559-572.
[Crossref] [Google Scholar] [PubMed]
- Dutta P, Giri S, Giri TK. Int J Biol Macromol. 2020; 160 (78): p. 55-68.
[Crossref] [Google Scholar] [PubMed]
- Almeida H, Amaral MH, Lobao P, et al. Drug Discov Today. 2014; 19(4): p. 400-412.
[Crossref] [Google Scholar] [PubMed]
- Irimia T, Dinu-Pirvu CE, Ghica MV, et al. Mar Drugs. 2018; 16(10): p. 373-375.
[Crossref] [Google Scholar] [PubMed]
- Majeed A, Khan NA. J Drug Deliv Ther. 2019; 9(1): p. 337-447.
- Khule MR, Vyavahare SB. Int J Res Educ Sci Met. 2021; 9(3): p. 899-909.
- Li J, Liu H, Liu LL, et al. Chem Pharm Bull. 2014; 62(10): p. 1000-1008.
[Crossref] [Google Scholar] [PubMed]
- Morsi N, Ghorab D, Refai H, et al. Int J Pharm. 2016; 506(1-2): p. 57-67.
[Crossref] [Google Scholar] [PubMed]
- Al Khateb K, Ozhmukhametova EK, Mussin MN, et al. Int J Pharm. 2016; 502(1-2): p. 70-79.
[Crossref] [Google Scholar] [PubMed]
- Qian Y, Wang F, Li R, Zhang Q, Xu Q. Drug Dev Ind Pharm. 2010; 36(11): p.1340-1347.
[Crossref] [Google Scholar] [PubMed]
- Ammar HO, Salama HA, Ghorab M, et al. Drug Dev Ind Pharm. 2010; 36(11): p. 1330-1339.
[Crossref] [Google Scholar] [PubMed]