Short Communication - Der Pharma Chemica ( 2021) Volume 13, Issue 7
Face masks: benefits and hitches amidst Covid-19 pandemic
Shailey Singhal1*, Shilpi Agarwal1, Kanchan Bahukhandi2 and Naveen Singhal32Department of HSE, School of Engineering, Energy Acres Building, University of Petroleum & Energy Studies (UPES), Bidholi, Dehradun-248007, Uttarakhand, India
3Department of Chemistry, DIT University, Village Makkawala, Dehradun-248009, Uttarakhand, India
Shailey Singhal, Department of Chemistry, School of Engineering, Energy Acres Building, University of Petroleum & Energy Studies (UPES), Bidholi, Dehradun-248007, Uttarakhand, India, Email: shailey@ddn.upes.ac.in
Received: 01-Jun-2021 Accepted Date: Jul 19, 2021 ; Published: 26-Jul-2021
Abstract
Covid-19 has aroused as the most contentious issues worldwide in 2020. It has caused unexpected effects on various aspects of life, and Governments are struggling in combatting this disease with all the efforts and measures possible at individual as well as mass scale. Various preventive measures have been recommended, including the use of face-masks for this purpose. This communication presents front and flip sides of using face-mask as a preventive measure. Health effects caused because of using face masks have been provided attention. Impact of quantification of face mask dumping is presented, along with a value added mechanism for the disposal of used masks as medical waste.
Keywords
Face-mask, Covid-19, healthcare workers, side effects, disposal of used face masks, thermal degradation
Introduction
Personal hygiene is of utmost importance for prevention against transmission of infectious viruses, especially in case of contagious respiratory diseases, such as influenza, severe acute respiratory syndrome (SARS), etc. And, this becomes even more important for healthcare workers (HCWs), who are exposed to such types of infections with maximum possibility and intensity. All the countries across the globe have attempted various measures and have issued necessary precaution to minimize the spread of Covid-19. This includes social distancing as first and foremost step towards prevention from the infection. Other necessary measures include use of hand sanitizers, frequent cleaning of hands, face- masks, face-shields, personal protective equipment (PPE; especially for healthcare and public workers), gloves, etc. Among variety of measures, face-masks have come up as necessary and important utility in this context, especially in the current scenario of Covid-19 pandemic. Corona virus is an acute respiratory syndrome virus and is responsible for respiratory illness linked to 2002-2003 outbreak (SARS-CoV-2) [1]; interestingly both the viruses have originally come from bats [2].
Covid patients include fever, cough, breathing problem and fatigue, however it has been observed to be highly contagious leading to severe complications, such as damage of important body organs (lungs, liver, heart). It can cause permanent loss of taste and smell, blood clotting, stroke, and finally death of the person. These are common symptoms observed in this illness, however extent of the infection can vary from person to person [3]; chronic illness and weak immune system further adds to the impact of attack on body [4,5].
Covid-19 (corona virus disease 2019) emerged during December 2019 in Wuhan, China, has turned up in pandemic. According to World Health Organization (WHO) data, captured on 20th May 2021, it has taken >165 million people across the world in its grip, and has resulted in >3 million fatalities round the globe [6]. There are number of ways in which this virus can be transmitted from one person to another, viz. simply by touching, speaking, sneezing, coughing, and breathing. Single coughing or sneezing expels out thousands of micro-organisms, which causes the virus to be spread in the form of aerosol, which travels the respiratory tract to affect the human beings [7-12]. The crucial thing in this process is the spread of virus via tiny droplets till many feets and remains active and live for number of days, however depends upon the size of the droplet also. For example larger droplets (>5μm) travels only up to <1 meter and remains in air for short time, while aerosolized droplets (<5μm) travel up to >1 meter and can exist in air for relatively long duration (around 3 hours); duration of its existence also varies on various surfaces [5, 13-17].
Face-masks as preventive measure
Prior to Covid-19 also, world has faced number of pandemics caused due to spread of viruses responsible for respiratory diseases; important ones being 2009 influenza, Ebola virus [18], avian influenza [19], and Middle East respiratory syndrome coronavirus (MERS-coronavirus) [20-21]. Pandemic strains generally have different transmission characteristics than seasonal strains, however both types vary with the age group involved too [22]. Controlling respiratory infections by using face- masks is a well-recognized measure. Masks prevent infection by trapping the moisture droplets coming out during speaking, sneezing and coughing [14, 23-24]. Use of masks is a subject of research on understanding the severity of transmission, especially when the transmission is observed to be air-borne; however the impact of implementing it as a preventive tool is quite visible in case of pandemic. Few countries have discouraged the use of face masks for the population, which has not been affected by Covid-19, however other countries encourage its usage [25-30]. Few reports state the recommendation of masks only in condition of illness, as its unnecessary usage creates a false sense of security in people, which increases the possibility of frequent touching of face and open areas of the body [26]. Team of researchers from Texas A&M University strongly recommends the use of masks in decreasing SARS- CoV-2 infection exponentially. Centre for Disease Control and Prevention (CDC) and World Health Organization (WHO) are also in complete agreement of this recommendation.
Studies indicate the reduction in the number of infected people by adopting face covering, both by masks and shields, as the single protective measure. A recent study indicates that this measure could prove helpful in reducing the number of infections by >78,000 in Italy (from 6th April to 9th May 2020) and by >66,000 in New York city (from 17th April to 9th May 2020) [31]. Another similar study shows the reduction of Covid-19 cases between 2.3-13% over 10 days in Germany on making face-masks compulsory to put on [32].
Indeed, the face-masks are more effective, where it is used regularly as a part of their routines [23, 33]. This is known as public masking, and studies indicate its effectiveness in preventing the spread of corona infection exponentially [34-35]. Public masking has been a cultural practice only in few Nations earlier, such as Japan, where it originated when it struggled with Spanish flu outbreak in 1918. Wearing mask is considered as a sense of security there. Similar few other Asian countries, such as China and South Korea are in regular practice of face masking. Now, under the increasing impact of Covid-19, it has become popular among majority of areas in around the globe, however percentage population is varying from one Nation to other. For example, citizens in few countries are still using it to a very lower extent than expected, like France (34%), Canada (28%), Australia (21%), Germany 20%) and the United Kingdom (16%). On the other hand, in other countries, people are well aware and motivated to use mask for the protection of self and others, like Spain (62%), India (76%), Japan (77%), Italy (81%), China (83%), and Vietnam (91%). A sharp increase has been observed in the mask users in United States from 11% (12-14th March 2020 - 9-12th April 2020) to 50% [36]. There have been certain claims, which are probably responsible for the lesser extent of public masking:
• Masks offer no protection to the wearer as masks are not the appropriate method to prevent the spread of SARS-CoV-2 virus, only N95 are the effective measures.
• Masks may increase risk of infection as masks can become contaminated very quickly, and every time the wearer breathes in, they inhale contaminants.
• Masks may harm the wearer as masks limit oxygen intake and increase carbon dioxide (CO2), and they increase the potential risk of CO2 poisoning.
Moving with these claims, a question obviously arises in the minds of public: ‘should we wear mask or not?’ So, to answer this, Governments, medical associations, organizations and all the governing bodies at any level have designed policies for the use of face-mask. Complete ‘No’ is not feasible for face- masks in the situation of this pandemic, and even under spread of any such infection, but policies need to be followed with precautions recommended, detailed in upcoming section of this paper.
Types of face-masks
Variety of face-masks are being used by the end user, governed by various factors, including professional requirement, livelihood status, availability, etc. Surgical masks, non-fit-tested P2 masks,home-made masks, 3-layered mask, synthetic masks, etc. are more common types to be used for such purposes (Figure-1).
N95 masks
N95 (American standard; equivalent to FFP2 in Europe) is basically a respirator, inbuilt with the provision to filter out aerosols and foreign particles [11]. It is named so because it is designed to stop 95% small foreign particles to enter the nose and mouth, if fitted properly. These are made up of polypropylene and the filtration efficiency & breathing resistance of these masks are governed by strict regulations, which also involve the shape and formation of masks in such a way that these provide perfect fit to users’ face. Owing to the very small pore size, these masks are extremely efficient, and are highly recommended for healthcare workers [37, 38]. If applied for proper sterilization, this type of masks can be made reusable, which will help in reducing the scarcity of their availability [39].
Surgical masks
Surgical masks are made up of polypropylene and largely used by medical practitioners, so are also referred to as ‘medical masks’. These are approved by the Food and Drug Administration (FDA) for being used in medical services and are relatively loose-fitting disposable masks. Being made up of polypropylene, these are efficient for preventing inhalation of larger droplets, however do not filter out airborne particles of sub-micron size [36, 40] produced via sneezing or coughing. Controversial statements have been found about the efficacy of surgical masks; at few places it has been reported to be sufficient enough, if used properly, while at few places, it has been quoted to around 90% efficient for stopping the transmission [27].
Cloth masks
Cloth masks are simple and economic means of replacing N95 and surgical masks, which people can stich at their own also, thus are very common to be employed in developing countries. Originally, cloth masks were only used to protect HCWs from infections [41, 42], later on in around 19th century, these were replaced by surgical masks, and then by respirators [43]. Keeping in view the cost and availability of N95, surgical and other specified masks, use of simple and economic cloth masks is strongly recommended as a means of transmission control. Cloth masks are effective in stopping the infection [34-35], and it is interesting to know that these are proved to be more effective than N95 and surgical masks [14-15]. However, another study from Duke University states that N95 respirators are most effective followed by three-layered surgical masks and consequently cloth mask made of a combination of cotton and polypropylene [44], which find agreement with lot of other studies also. Cloth masks are generally multi-layered with fixed ear loops, and their filtration ability depends upon the type and layers of fabric fixed in it [45-47]. The filtration ability of cloth masks is governed by various parameters of cloth which is used to prepare masks, such as pore shape, pore size, pore number density and clearance [48]. Commonly available cloth masks display filtration rate of 49-86% for 0.02 μm exhaled particles [49]. Regular washing and drying also affects its filtration ability. Although evidences are reported, but the effectiveness of cloth masks is a subject of discussion as references also indicate about their in-suitability, which might be due to their continuous and repeated use without proper sterilization [50,51]. Due to increase moisture retention, virus may survive on the surface of masks, leading to self-contamination. A detailed study conducted by Mitze et al. (2020) on HCWs indicates that the rate of infection has been lowest while using medical masks while highest in case of cloth masks [32]. Perhaps, this is the reason why cloth masks have rarely been recommended in policy documents [41-42], and also have not been attempted for randomized clinical trials (RCTs) [50].
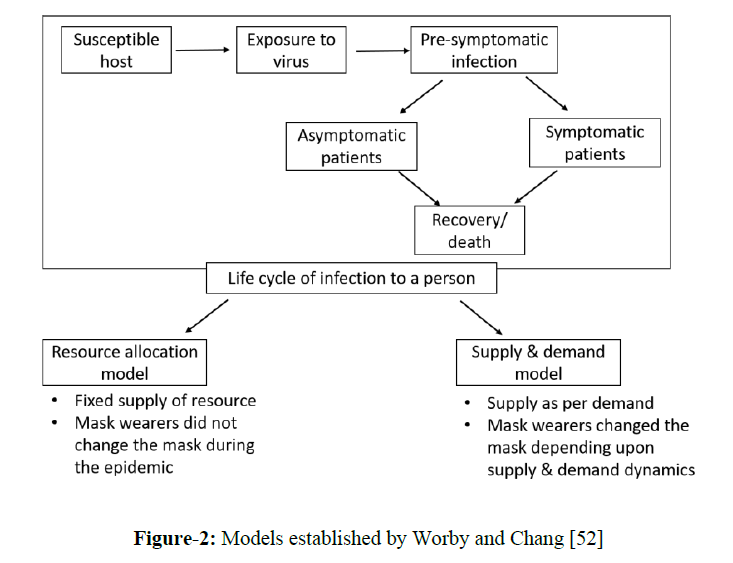
Worby and Chang (2020) [52] studied the effect of face mask distribution and usage to understand its role in reducing the number of infections and deaths due to Covid, optimizing distribution in resource- limited setting, and role of demand and dynamic supply of face masks. They established two models for this purpose: (1) ‘reuse allocation model’, in which limited number of masks could be distributed among people, and (2) ‘supply and demand model’, in which mask production rate and its dynamic supply was captured (figure-2). Applying various strategies of distributing the masks to the infected population, they observed that (1) targeted distribution of masks in limited resource could decrease the death rate, (2) optimal distribution helps in controlling the situation to a better level, (3) panic buying increases illness, and (4) universal face covering in public is helpful in reducing the number of infected cases to a greater extent.
Figure 2: Models established by Worby and Chang [52]
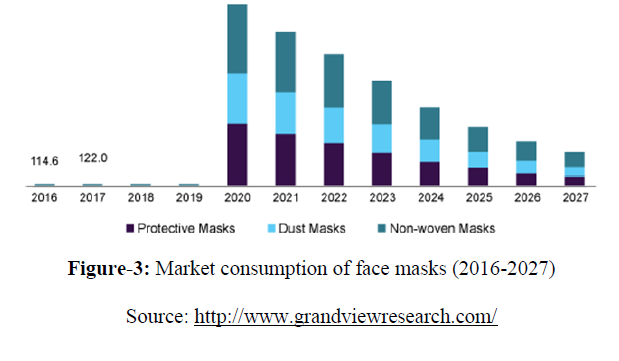
Covid pandemic has impacted disposable face mask market to an unexpected extent. The 3M Company (US), Honeywell International Inc. (US), Kimberly-Clark (US), Owens & Minor, Inc. (US), and Cardinal Health, Inc. (US) are few key market players leading the face mask industry. Recently, in August 2020, Honeywell International Inc. (US) has established Fulgaon manufacturing facility at Pune (India) for the production ~2 million disposable face masks/ month. The global market size for disposable face masks has exceeded USD 74.90 billion in 1st quarter of 2020, and is expected to increase at a compound annual growth rate (CAGR) of 53% till 2027 (figure-3) [53].
Figure 3: Market consumption of face masks (2016-2027)
Handling of face masks
Number of measures are being recommended and taken all over the world to minimize the number of people affected from it, which includes social distancing, sanitizers, isolation, face-masks, face shields, PPE kits, etc. Social distancing, sanitizers and isolation decreases direct contact, but is not able to prevent air borne transmission. On the other hand, face covering is quite effective in preventing air borne transmission also by blocking the shedding and spreading of sneezing/ coughing droplets. An important concern is regarding wearing the mask properly; as many a times it is possible that infection, accumulated on the outer surface of mask, in the form of bacteria or virus, can be transferred to hands, which can become its carrier to mouth or eyes, and finally inside the body [54,55]. Proper donning and removal of face mask is important for providing effective protection to the user [56]:
• Performing hand hygiene before wearing and removing the mask.
• Choosing appropriate size of mask.
• Touching only the elastic bands while using it.
• Avoiding touching the mask, once it is properly fit at mouth and nose.
• In case mask becomes wet or dirty, change it with the clean one.
• Keep the dirty/ wet mask in a sealable bag till it is not washed.
• Removal of mask should be chin upwards.
• Folding the mask half inward after taking off, and then again folding it half inward to make its roll before disposing off.
• Disposing the mask properly in plastic/ paper bag in covered bin.
Mask should be perfectly fit at the face and should have no openings from the sides; else instead of decrease, an increase in spread of respiratory infection can also be there [57, 58]. Masks should be washed daily, preferably in hot water. Other methods for cleaning the masks include the use of isopropyl alcohol or hydrogen peroxide, and bleach. Exposure to ultraviolet (UV) radiations, dry heat, microwave and autoclave helps in sterilizing the masks [59].
Efficacy of face coverings: Side effects of using face coverings
Utilizing face-masks and coverings does not need any proof as these are in continued use for centuries by medical practitioners and scientists in sophisticated labs [8-63]. They are safe to use, however certain side effects also remain associated with it [64-66]. The side effects associated with the use of face masks vary in the severity of problem. This includes discomfort, rashes, skin irritation, headache, etc. [67]. Headache is more common in case of donning N95 [68]. The discomfort and its intensity in the users is due to varied reasons, such as physical exertion, environmental factors (temperature, ventilation, size of residing area), and the proper size of mask. It also depends upon the individual daily accessories, like, eye glasses, and facial structure as well. Situation is more difficult for the patients experiencing acute pre-existing renal disease, as wearing N95 for long time may result in breathing difficulty in them [69].
For patients with chronic obstructive pulmonary disease (COPD), breathing becomes difficult in the presence of mask; also it causes exhaled carbon dioxide to be inhaled again. These factors increase the frequency and deepness of breathing [70]. In continuation to above, persons with physical disabilities are not advised to use face-masks as they cannot adjust their mask [24]; also people with respiratory diseases and the children below age of 2 years should not use mask [69]. Li et al. has deeply investigated the impact of wearing surgical and N95 masks on the health of the subjects under investigation [71]. As a result of their experiments, they concluded that both surgical and N95 masks induce different temperature and humidity in the microclimates of face masks, which caused profound effects on heart rates and thermal stress of the patient. Variation in temperature inside the face mask creates local thermal stimulus to the skin around the mouth, nose and cheeks. This causes heat exchanges from the respiratory tract [72], creating breathing resistances. Due to shortage of oxygen, sympathetic nervous system and increased heart rate is experienced [73]. Ill effects on the physiology of body, such as breathing resistance, itching, fatigue, discomfort, etc. is even more prominent in N95 as compared to surgical masks [74]. Effect of donning the masks on health of a person has been studied by several other workers also [75-78]. Presence of exhaust valve has been recommended to be effective in reducing the temperature and humidity inside the mask, accelerating dry and wet heat loss through the nose [79]. Other common problems observed are headaches, acne, and change in skin pigments, dryness and rashes on skin, causing irritation [80].
Certain common behavioural measures have been suggested to prevent from the side effects caused by wearing face-masks. Drinking plenty of water, eating fresh vegetables and fruits is common prevention. Using moisturiser, body wash and cream can be helpful in overcoming skin problems. Anti-fungal dusting powders are useful in preventing fungal infection caused. Along with this, breathing protocol, as recommended by PN Medicals, should be adopted while wearing face-mask. This includes performing five quality breaths prior to putting on mask, immediately after putting it on and when it is removed. Quality breath is referred to as four seconds of breathing in through the nose, six seconds of exhaling through the mouth and pausing two seconds before repeating. This helps in preventing dysfunctional breathing pattern. Longer and slower breaths should be practised while wearing a mask. Respiratory Muscle Training (RMT) should be practized for five minutes in the morning and five minutes in the evening using a clinically proven device such as The Breather by PN Medical.
Disposal/ Recycling of used masks
Despite of advantage of using face masks in preventing respiratory diseases, used masks are treated as medical waste and as per guidelines issued by Government. Disposed masks pose potential social and environmental risks, and need careful disposal in a rubbish bag (zip-locked bag), which in turn should be kept in another rubbish bag, tied it properly, and should be kept separate from other waste; else, there is a possibility of their re-use or recycling after picking up back. In any case, it should not be thrown open at road sides or in dust bins. Although this method of disposal simply leads to the increasing the pile in dumping area. The important thing is that disposable masks come under the category of one- time used plastic, which is a menace to the environment. Currently millions of contaminated non- recyclable masks are dumped as the irreversible infectious waste, affecting environment and human health in a devastating manner. Sangkham (2020) [81] utilized following equation as suggested by Nzediegwu and Chang [82] for the estimation of face mask consumption by people in Asian region:
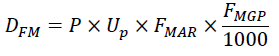
Where,
DFM: Daily face mask use (piece)
P: Population of people
Up: % of urban population
FMAR: Face masks acceptance rate (80%)
FMGP: Assumption that each person under observation uses one face mask per day [83]
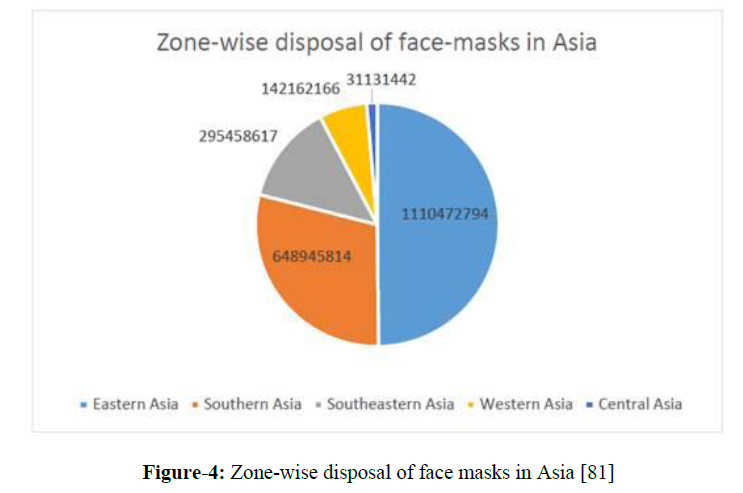
He evaluated the scenario of 49 Asian countries and estimated that a total of 2,228,170,832 face masks were used and thrown in all the selected countries. Details of few countries with disposal guidelines are presented in table-1. Zone-wise disposal of face-masks in Asia is represented in figure-4 [81]. The estimation was based upon the total population, percentage of urban population, percentage of face mask acceptance rate, and daily face mask consumption per person (assumed to be one).
| Country | Total population | Urban population | Number of Covid cases | Number of face masks used/ day | Recommended disposed face mask management | Reference |
|---|---|---|---|---|---|---|
| China | 1,439,323,776 | 86 | 84,292 | 989,103,299 | Collection in special trash cans/ plastic wrapping before disposal Medical masks used by healthy people to be disposed off with domestic waste Special masks and gloves to be used by sanitation workers while disposing garbage bags, disinfecting bins, and keeping garbage bags in collection vehicle Vehicles need to be sealed and sterilized before entering and leaving a community |
[84-85] |
| India | 1,381,085,714 |
35 | 1,643,416 | 381,179,657 | To wrap used masks in paper bag for 72 hrs before disposal To be strapped into pieces before disposal To disinfect the masks with 5% bleach solution or 1% hypo solution, followed by incineration by Greater Chennai Corporation (GCC) |
[86] |
| South Korea | 51,272,891 | 36 | 14,305 | 14,561,501 | To dispose in garbage bag labelled ‘Waste for incineration’ and ‘Waste bag for landfill’ Segregation by volume-based waste fee (VBWF) system before transportation to recycling facilities Incineration of disposal in landfills without recycling |
[87] |
| Thailand | 69,814,554 | 18 | 3,310 | 10,220,851 | Placement of special red bins labelled ‘For used face mask only’ in highly visible areas by Bangkok Metropolitan Administration (BMA) To keep in Ziploc bags by household before disposal in red bins To keep special bins in waste collection vehicles To label the bag with ‘HW’ in case red bins are not available around Incineration at specialist facilities in Nong Khaem and On Nut |
[88-90] |
| Taiwan | 23,820,377 | 37 | 467 | 7,050,832 | Folding mask in half with contaminated side inwards in case of reusing the mask Lidded trash can to be used for disposal Mandatory wearing of face mask in public Fine of 122 USD for improper disposal under The Waste Disposal Act by Environmental Protection Administration |
[91-92] |
| Malaysia | 32,398,441 | 27 | 8,964 | 7,049,901 | Hygienic disposal by folding the mask with contaminated part inwards, rolling it up, wrapping in plastic and placing in rubbish before disposal collection by Kepong MP Lim Eng. |
[93] |
| Singapore | 5,854,053 | 93 | 51,809 | 4,364,782 | To be treated as ordinary non- contaminated municipal waste Disposal in residential and public areas |
[94] |
Table 1: Face masks disposed off in various countries and preventive guidelines
Figure 4: Zone-wise disposal of face masks in Asia [81]
Countries generating so much high amount of face mask as medical waste should give a proper concern to its safe management, including collection, transportation, segregation, pre-treatment, storage, and disposal. Few countries have issued guidelines for this purpose, concerning socio-economic conditions and technologies available (table-1). Permanent solution to discard this kind of waste is to incinerate the used cloth mask, contaminated with infected droplets and germs in electrical incinerators available in market. This is a biologically safe process, where used masks are incinerated at 1100°C for 3 minutes [95-96].
Special consideration needs to be given to N95 and surgical masks, made up of polymeric propylene (PP)/ urethane (PU)/ esters. These come under the category of single used plastic, leading to severe environmental consequences. It is estimated that during the peak of Covid in Wuhan alone, >240 tons of medical waste was generated per day, including appreciable amount of face masks in it [97]. Recent studies estimate that 129 billion face masks are thrown in garbage globally every month, most of which are made from plastic microfibres [98-99]. Being contaminated with micro-sized germ particles, these are even more dangerous than regular plastic waste.
It is well explored that these polymeric materials, especially polypropylene cannot be decomposed easily due to high hydrophobicity, high molecular weight, no functional group at the surface. These properties simply cause its accumulation in the environment, which causes the gradual generation of large number of nano-sized polypropylene particles (<1mm) due to in-situ weathering [100].
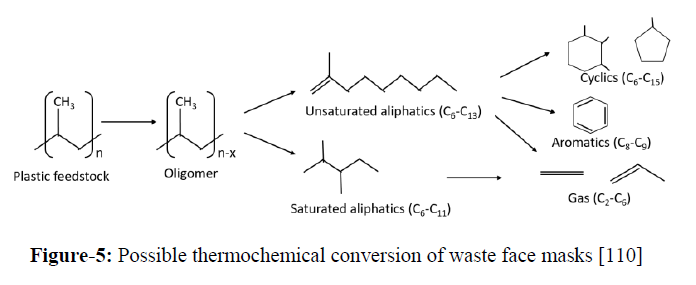
A scientific and feasible solution is necessary to address the waste generated by disposal of polymer based face masks. These can be subjected to thermal cracking and pyrolysis under controlled conditions, which converts this material to liquid hydrocarbons with preponderance in gasoline to diesel range hydrocarbons and other petrochemicals of industrial significance (figure-5) [101-110].
Figure 5: Possible thermochemical conversion of waste face masks [110]
Supercritical water depolymerisation can be a suitable choice for managing polyolefin waste, as it is carried out under moderate temperature/ pressure without utilizing any catalyst, and generate high quality products. Recently, Chen et al. [111] have converted polypropylene to gasoline range hydrocarbon oil using supercritical water at 380-500°C for 0.5-6hrs at 23 MPa. The hydrocarbon oil obtained was comprising the calorific value 48-49MJ//kg. Thus, thermochemical conversion can be presented as sustainable solution for managing this menace after sterilization.
Conclusion
Due to contradictory reports and ambiguous guidelines, use of masks is a matter of discussion to be used in case of infectious diseases. Policy makers need to take decisions and issue guidelines for proper usage of face-masks clearly under varying conditions of infections. Guidelines are also required for production, distribution and sanitization procedures of masks for their effective usage for prescribed duration. Proper disposal of face-masks also needs concern and attention by Governments to allow its acceptance and implementation. Thermochemical conversion of face masks to liquid fuels and value added petrochemicals seems to be an effective and sustainable route to dispose off face-masks, while converting it to liquid fuels. This will not only manage the problem of waste management, but will also serve as an important step towards producing energy and securing the environment.
References
- Fehr AR and Perlman S, Methods Mol. Biol., 2015. 1282: p. 1–23.
- Cohen J, American Association for the Advancement of Science, 2020.
- Xu Z, Shi L, Wang Y et al., the Lancet Respiratory Medicine, 2020. 8: p. 420–422.
- Peter PL, Alice B, David S et al., Circulation, 2020. 142: p. 68–78.
- Contini D and Costabile F, Atmosphere, 2020. 11: p. 377-381.
- https://Covid19.who.int/, 2021.
- Kutter JS, Spronken MI, Fraaij PL et al., Curr. Opin. Virol., 2018. 28: p. 142–151.
- Leung NHL, Chu DKW, Shiu EYC et al., Nat. Med., 2020. 26: p. 676–680.
- Stadnytskyi V, Bax CE, Bax A et al., Proc. Natl. Acad. Sci. 2020. 117: p. 11875–11877.
- Zhang R, Wang G, Guo S et al., Chem.Rev., 2015. 115: p. 3803-3855.
- Howard J, Huang A, Li Z et al., Preprints, 2020.
- Qian G, Yang N, Ma AHY et al., Clin Infect Dis, 2020. 71: p. 861-862.
- Lu J, Gu J, Li K et al., Emerging infectious diseases, 2020. 26: p. 1628-1631.
- Anfinrud P, Stadnytskyi V, Bax CE et al., N Engl J Med, 2020. 382: p. 2061–2063.
- Verma S, Dhanak M and Frankenfield J. Physics of Fluids, 2020. 32: p. 061708.
- van N Doremalen, Morris DH, Holbrook MG et al., N Engl J Med, 2020. 382: p. 1564–1567.
- Bourouiba L, JAMA, 2020. 323: p. 1837–1838.
- World Health Organization (WHO), http://www.who.int/csr/don/2014_08_28_ebola/en/, 2014.
- World Health Organization (WHO), http://www.who.int/csr/don/2013_05_07/en/index.html, 2013.
- Bermingham A, Chand MA, Brown CS et al., Euro Surveill, 2012. 17: p. 20290.
- Pollack MP, Pringle C, Madoff LC et al., Int J Infect Dis, 2013, 17: p. e143–144.
- MacIntyre CR, Dwyer SCDE, Seale H et al., Emerging Infectious Diseases, 2009. 15: p. 233-241.
- Tam VC, Tam SY, Poon WK et al., E Clinical Medicine, 2020. 22: p. 100356.
- Desai AN and Aronoff DM, JAMA, 2020. 323: p. 2103.
- Buchwald E, marketwatch. 2020.
- Little S, https://globalnews.ca/news/6486026/bc-cdc-coronavirus-misconceptions/., 2020.
- Lopez ML, CNN Philippines., 2020.
- Shen M, Peng Z, Xiao Y et al., bioRxiv., 2020.
- Wernau J and Xie SY, The wall street journal. 2020.
- The Jakarta Post, Health ministry official. 2020.
- Zhang R, Li Y, Zhang AL et al., PNAS, 2020. 117: p. 14857–14863.
- Mitze T, Kosfeld R, Rode J et al., IZA Institute of Labor economics, 2020.
- ]Goldman Sachs Research, 2020
- Wang X, Ferro EG, Zhou G et al., JAMA, 2020. 324, p. 703-704.
- Hendrix MJ, Morb Mortal Wkly Rep, 2020. p. 69.
- Science daily, https://www.sciencedaily.com/releases/2020/06/200612172200.htm, 2020.
- MacIntyre CR, Wang Q, Cauchemez S et al., Viruses, 2011. 5: p. 170-179.
- MacIntyre CR, Wang Q, Seale H et al., Am J Respir Crit Care Med, 2013. 187: p. 960–966.
- de Man P, van Straten B, van den Dobbelsteen J et al., J Hosp Infect, 2020. 105: p. 356-357.
- Migliori GB, Nardell E, Yedilbayev A et al., Eur Respir J, 2019. 53: p. 1900391.
- Chughtai AA, Seale H and MacIntyre CR, Int. J. Infect. Control, 2013. 9: p. 1-12.
- Chughtai AA, Seale H and MacIntyre CR, BMC Res Notes, 2013. 6: p. 1–9.
- Quesnel LB, Br J Surg, 1975. 62: p. 936–940.
- Fischer EP, Fischer MC, Grass D et al., Science Advances, 2020.
- Konda A, Prakash A, Moss GA et al., ACS Nano, 2020. 14: p. 6339–6347.
- Mueller AV, Eden MJ, Oakes JM et al., medRxiv., 2020.
- Rengasamy S, Eimer B and Shaffer RE. Ann Occup Hyg, 2010. 54: p. 789–798.
- Neupane BB, Mainali S, Sharma A et al., Peer J, 2019. 7: p. e7142.
- Davies A, Thompson KA, Giri K et al., Disaster Medicine Public Heal. Prep., 2013. 7: p. 413–418.
- MacIntyre CR and Chughtai AA, BMJ, 2015. 350: p. h694.
- Offeddu V, Yung CF, Low MSF et al., Clinical Infectious Diseases, 2017. 65: p. 1934-1942.
- Colin J. Worby & Hsiao-Han Chang. Nature communications, 2020. 11: p. 4049-4057
- Market analysis report, 2020-2027., grandviewresearch, 2021.
- MacIntyre CR, Zhang Y, Chughtai AA et al., BMJ Open, 2016. 6: p. e012330.
- Abd-Elsaye A and Karri J, Anesth Analg, 2020. 131: p. 4–6.
- Lee LY, Lam EP, Chan C et al., BMC Public Health, 2020. 20: p. 948-958.
- World Health Organization (WHO), 2009.
- World Health Organization (WHO), http://www.who.int/csr/don/2009_11_27a/en/index.html, 2009a
- Institute of Medicine, Washington (DC): The National Academies Press, 2006.
- Oberg T and Brosseau LM, Am. J. Infect. Control, 2008. 36: p. 276–282.
- Long Y, Hu T, Liu L et al., J Evidence-Based Medicine, 2020. 13: p. 93–101.
- Atkinson J, Chartier Y, Pessoa-Silva CL et al., World Health Organization, 2009.
- Brenner AM, Weiser PC, Krogh LA et al., JAMA, 1980, 244: p. 2196–2198.
- Greenhalgh T, Schmid MB, Czypionka T et al., BMJ, 2020. p. 369.
- Lim ECH, Seet RCS, Lee KH et al., Acta Neurologica Scandinavica, 2006. 113: p. 199–202.
- Roberge RJ, Coca A, Williams WJ et al., Respirology, 2010. 15: p. 516–521.
- Luo P, Liy D and Li J, Dermatologic Therapy, 2020. 33: p. e13745
- Jacobs JL, Ohde S, Takahashi O et al., Am. J. Infect. Control, 2009. 37: p. 417–419.
- Kao TW, Huang KC, Huang YL et al., Med. Assoc., 2004. 103: p. 624–628.
- Kyung SY, Kim Y, Hwang H et al., Respir Care, 2020. 65: p. 658-664.
- Li Y, Tokura H, Guo YP et al., Int Arch Occup Environ Health, 2005. 78: p. 501–509.
- Nielsen R, Berglund LG, Gwosdow AR et al., Ergonomics, 1987. 30: p. 1689-1703.
- Ganong WF, Appleton and Lange, Stamford, 1997. 1703: p. 565–566.
- White MK, Hodous TK and Vercruyssen M. Ergonomics, 1991. 34: p. 445–457.
- Hayashi C, Iriki T, Nakayama T et al., 1988. 48: p. 49–55.
- Flaherty DK, Taylor PM, Hopkins WE et al., J Occup Environ Med, 1995. 37: p. 1116–1121.
- Alston S, Powell L, Stroud P et al., J Int Society for Respiratory Production, 1997. 15: p. 24–35.
- Desruelle AV and Candas V. Eur J Appl Physiol, 2000. 81: p. 33–39.
- Hayashi C and Tokura H, Int Arch Occup Environ Health. 2004. 77: p. 73–78.
- Rosner E. J. Infect. Dis. Epidemiol, 2020. 6: p. 130.
- Sangkham S., Case Studies in Chemical and Environmental Engineering, 2020.
- Nzediegwu C and Chang SX, Resour. Conserv. Recycl., 2020. 161: p. 104947.
- L H. Wu, Huang J, Zhang CJP et al., EClinicalMedicine, 2020. 21: p. 100329.
- Rongmeng J and Jianguo J, straitstimes. 2020.
- Wang J, ichongqing. 2020.
- Bandela DR, downtoearth. 2020.
- W S. Rhee, Waste Manag. Res., 2020. 38(8): p. 820–824.
- Ministry of Public Health, 2020.
- Pollution control department, 2020.
- Thampanishvong K and Wibulpolprasert K, Thailand Development Research Institute, 2020.
- www.taiwannews.com. 2020.
- Lee CE, Fight covid taiwan, 2020.
- Bavani M, metro-news, 2020.
- International Solid Waste Association, 2020.
- Kanemitsu K, Inden K, Kunishima H et al., J. Hosp. Infect., 2005. 60(4): p. 304–306.
- Di Maria F, Bidini G, Lasagni M et al., Appl. Therm. Eng., 2018. 129: p. 338–344.
- Sonia A and Kumar R. nepalitimes, 2020.
- Prata JC, Silva AL, Walker TR et al., Environmental Science & Technology, 2020. 54(13): p. 7760–7765.
- Xu EG and Ren ZJ, Front. Environ. Sci. Eng., 2021. 15(6): p. 125.
- Mattsson K, Jocic S, Doverbratt I et al., Amsterdam: Elsevier, 2018. p. 379–399.
- Ahmad I, Khan MI, Khan H et al., Int J Green Energy, 2015. 12: p. 663-671.
- Jin LE, Wang L, Su L et al., Int J Green Energy. 2012. 9: p. 719-730.
- Shah J, Jan MR and Mabood F, Energy Conversion and Management, 2009. 50: p. 991-994.
- Shah J, Jan MR and Mabood F, J Poly Env, 2007. 15: p. 207-211.
- Jan MR, Shah J and Gulab H, Fuel Processing Technology, 2010. 91: p. 1428-1437.
- Ali MF, Nahid M and Redhwi SSHH. J. Mater. Cycles Waste Manag. 2004. 6: p. 27-34.
- Ciliz K, Ekinci NE and Snape CE, Waste Management, 2004. 24: p. 173-181.
- Demirbas A, J Anal Appl Pyrolysis, 2004. 72: p. 97-102.
- Kodera Y, Ishihara Y and Kuroki T. Energy & Fuels, 2006. 20: p. 155-158.
- Miao Y, Von Jouanne A and Yokochi A, Polymers, 2021. 13: p. 449-466.
- Chen WT, Jin K and Wang NHL, Acs Sustain. Chem. Eng., 2019. 7: p. 3749–3758.