Research Article - Der Pharma Chemica ( 2021) Volume 13, Issue 9
Design, Synthesis and Evaluation of Benzothiazole Urea Derivatives as an Anticonvulsant Agent
Snehal D. Kachare1, Kamalkishor G. Baheti2, Qazi Yasar2 and Sampada S. Jangam12YB Chavan College of Pharmacy, RauzaBagh Aurangabad (MS) India -431001, India
Received: 28-Aug-2021 Accepted Date: Sep 24, 2021 ; Published: 30-Sep-2021
Abstract
A series of 1-((-6-substituted-2-yl)-3-(4H-1,2,4 triazole-3-yl)urea 7a-f and (1-((3-(6-substituted-2-yl)ureido)methyl)cyclohexyl)acetic acid 8a-fwere designed, synthesized using appropriate synthetic route and screened for CNS depressant and anticonvulsant activities. The synthesized compounds were also analyzed for ADME properties. The results of In-Silico ADME Screening showed that compounds could be exploited as an oral drug candidate. Molecular docking studies were performed for all the synthesized compounds against γ-amino butyric acid amino transferase enzyme (1OHV), All the compounds exhibited docking score in the range of -7.5 to -8.4, among which compound 8c had shown the highest docking scores as compared to the standard drug phenytoin. Animal study for anticonvulsant indicated that compounds 7b, 7e and 8c were exhibited significant activity at a dose 200 mg/kg. All these compounds were also evaluated for CNS depressant activity using actophotometer. The results of CNS depressant and anticonvulsant activities and docking study showed that synthesized compounds had potential CNS depressant and anticonvulsant activities and can be further optimized and developed as a lead compound.
Keywords
Benzothiazole, Urea derivatives, MES, Anticonvulsant, CNS depressants, Molecular modelling
Introduction
Epilepsy is a brain disorder characterized by seizures that have neurobiological, emotional, psychological and social implications. An epileptic seizure is a temporary event of signs and symptoms in the brain in which cells use chemical reactions to generate electric discharges due to abnormal, excessive or synchronous neuronal activity. Each brain cell and its discharges either excite or inhibit other brain cells. If the balance of excitation and inhibition is shifted too far in the direction of excitation in a region of the brain, the outcome could be a seizure [1]. Excitability is the most significant property of nerve cells. By producing an action potential, it responds to excitation, which can lead to repeated discharge. When subjected to excessive excitation due to brain injury, cerebrovascular disease, head trauma, drug or alcohol abuse, neoplasia, infection and genetic factors [2,3], all normal neurons can become epileptic. A research indicates that epilepsy is the third most progressive degenerative condition that affects 0.5-1% of individuals around the world. In India, epilepsy prevalence rates range from 1710 to 9780 cases per million populations [4,5]. Anti-epileptic drugs (AEDs) currently available have minimal effectiveness and can only offer symptomatic relief as these drugs inhibit seizures and have little effect on epileptogenesis, a process that turns the normal brain circuitry, even after an injury, into a hyper-excitable one. Due to their adverse effects, withdrawal symptoms, deleterious interactions with other drugs and economic burden, long-term use of antiepileptic drugs is limited , especially in developing countries [6-8]. Research work in the decade indicated that different heterocyclic rings have been studied for antiepileptic activity, but still the new drugs available in market are not able to fulfill all need that required during treatment [9]. There is lack of target specificity in the development of dependence and side effects. In the production of dependencies and side effects, there is a lack of target specificity. For experimental drug design, benzothiazole may serve as special and flexible scaffolds. Benzothiazole has a significant place among all benzoheterocycles in the research area, especially in synthetic and pharmaceutical chemistry, because of its potent and significant pharmacological activities. In recent years, heterocyclic compounds containing small and simple Benzothiazole and 1, 2, 4-triazole nucleus have attracted strong interest. These nucleus are found in biologically active compounds such as anti-tumor [10], anti-microbial [11], anti-tumor [12], anti-diabetic [13], anti-convulsant [14] and anti-inflammatory [15]. 2-Aminobenzothiazoles were intensively studied as central muscle relaxants [16].
Epilepsy is a brain disorder characterized by seizures that have neurobiological, emotional, psychological and social implications. An epileptic seizure is a temporary event of signs and symptoms in the brain in which cells use chemical reactions to generate electric discharges due to abnormal, excessive or synchronous neuronal activity. Each brain cell and its discharges either excite or inhibit other brain cells. If the balance of excitation and inhibition is shifted too far in the direction of excitation in a region of the brain, the outcome could be a seizure [1]. Excitability is the most significant property of nerve cells. By producing an action potential, it responds to excitation, which can lead to repeated discharge. When subjected to excessive excitation due to brain injury, cerebrovascular disease, head trauma, drug or alcohol abuse, neoplasia, infection and genetic factors [2,3], all normal neurons can become epileptic. A research indicates that epilepsy is the third most progressive degenerative condition that affects 0.5-1% of individuals around the world. In India, epilepsy prevalence rates range from 1710 to 9780 cases per million populations [4,5]. Anti-epileptic drugs (AEDs) currently available have minimal effectiveness and can only offer symptomatic relief as these drugs inhibit seizures and have little effect on epileptogenesis, a process that turns the normal brain circuitry, even after an injury, into a hyper-excitable one. Due to their adverse effects, withdrawal symptoms, deleterious interactions with other drugs and economic burden, long-term use of antiepileptic drugs is limited , especially in developing countries [6-8]. Research work in the decade indicated that different heterocyclic rings have been studied for antiepileptic activity, but still the new drugs available in market are not able to fulfill all need that required during treatment [9]. There is lack of target specificity in the development of dependence and side effects. In the production of dependencies and side effects, there is a lack of target specificity. For experimental drug design, benzothiazole may serve as special and flexible scaffolds. Benzothiazole has a significant place among all benzoheterocycles in the research area, especially in synthetic and pharmaceutical chemistry, because of its potent and significant pharmacological activities. In recent years, heterocyclic compounds containing small and simple Benzothiazole and 1, 2, 4-triazole nucleus have attracted strong interest. These nucleus are found in biologically active compounds such as anti-tumor [10], anti-microbial [11], anti-tumor [12], anti-diabetic [13], anti-convulsant [14] and anti-inflammatory [15]. 2-Aminobenzothiazoles were intensively studied as central muscle relaxants [16].
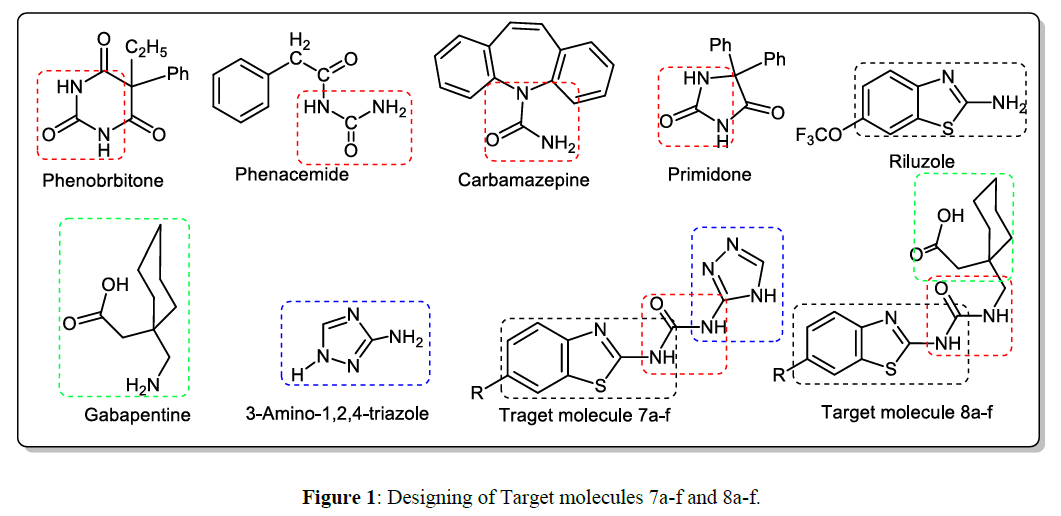
The design and synthesis of titled compounds were carried out with the objective to form a hybrid structure of two heterocyclic compounds with a pharmacophoric urea linkage for antiepileptic activity. Present study include the design and derivatization of Benzothiazole with gabapentin and 3- amino-1, 2, 4-triazole independently. All compounds were found to have log p in the range 2 to 4. Designed target compounds possess the log p value lower than 4 for crossing Blood Brain Barrier and also these derivatives showed good interactions with GABA-AT receptor in docking studies and exhibited dock score -7.5 to -8.4.
In some of the well-known anticonvulsant agents with various mechanisms, the N-C=O moiety is well known as a pharmacophoric requirement (Figures 1 and 2) [9]. Despite these facts and as part of our ongoing studies in this area, it was thought to synthesized urea linked hybrid analogue of benzothiazole with 3-amino-1,2, 4triazole and gabapentin independently for anticonvulsant and CNS depressant activity.
Materials and Methods
Experimental
General: All chemicals were obtained from Merck Ltd., India and used without further purification. The reactions were carried out by conventional method. Melting points were determined in open capillary using melting point apparatus and are uncorrected. The purity of synthesized compounds was ascertained by TLC using silica gel-G pre-coated plate (Merck, Germany) as a stationary phase and iodine vapors and UV lamp for visualization of spot. The elemental analysis (C, H, and N) of all compounds was performed on Germany's Vario EL III (HNS Elimentar Analyser system, GmbH) and results were within ± 0.4% of the theoretical values. IR, 1H-NMR and Mass spectral analysis performed to ascertain the structures of synthesized compounds. The IR spectra were recorded in a KBr disc and the absorption spectra are expressed in cm-1 on a Bruker spectrophotometer. The 1H-NMR spectrum was recorded on a CDCl3 / DMSO-d6 Varian AS 400 MHz spectrometer. Chemical shifts (δ) (in ppm) are relative to TMS. Mass spectra were taken on a Macro mass spectrometer (Waters) by electro-spray method (ES).
General procedure to synthesize of 1-(6-substituted benzothiazol-2-yl)-3-(4H-1, 2, 4-triazol-3-yl) urea (7a-f): Ethyl-6-substituted benzothiazol-2-ylcarbamate 4a-f (0.005 mol) and 3-amino-1,2,4- triazole(5) (0.005 mol, 0.252 g) was transferred independently to 100 ml RBF. To this solution, 15 ml methanol was added and refluxed for 3 h at 60-70ºC. Completion of reaction was monitored by TLC. After completion of reaction, the mixture was poured on crushed ice and stirred. Product was precipitated out and it was filtered and dried. Recrystallised from ethanol to obtained pure compounds 7a-f. Physicalcharacterization data was given in Table 1
| Compound | R | Molecular formula | Molecular Weight | m. p. °C | % Yield |
|---|---|---|---|---|---|
| 7a | CH3 | C11H11N6OS | 275 | 275-276 | 72.99 |
| 7b | NO2 | C10H7N7O3S | 303 | 256-257 | 66.66 |
| 7c | Cl | C10H7N6OSCl | 294 | 237-238 | 69.38 |
| 7d | OCH3 | C11H10N6O2S | 290 | 283-284 | 67.58 |
| 7e | H | C10H8N6OS | 260 | 129-130 | 68.46 |
| 7f | SO2NH2 | C10H9N7O3S | 307 | 268-269 | 61.88 |
| 8a | CH3 | C17H23N3O3S | 349 | 228-230 | 64.18 |
| 8b | NO2 | C17H20N4O5S | 392 | 248-250 | 63.77 |
| 8c | Cl | C17H20N3O3SCl | 381 | 280-282 | 64.66 |
| 8d | OCH3 | C18H23N3O4S | 376 | 212-214 | 65.20 |
| 8e | H | C17H21N3O3S | 347 | 173-174 | 67.72 |
| 8f | SO2NH2 | C17H22N4O5S2 | 426 | 278-279 | 68.07 |
Characterization data for 1-((-6-substituted-2-yl)-3-(4H-1,2,4 triazole-3-yl)urea (7a-f )
General procedure to synthesize 2-(1-((3-(6- methylbenzothiazol-2-yl)ureido) methyl) cyclohexyl) acetic acid (8a-f): Ethyl-6-substituted benzothiazol-2-ylcarbamate 4a-f (0.005mol) and gabapentin (7) (0.005 mol) was transferred independently to RBF (100 ml). To this solution, 15 ml methanol was added and refluxed for 2.30 h at 60-70°C. Completion of reaction was monitored by TLC. After completion of reaction, the mixture was poured on crushed ice and stirred. Product was precipitated out and it was filtered and dried. Recrystallized from ethanol to obtained pure compounds 8a-f. Physical Characterization data was given in Table 1.
1-(6-Methylbenzothiazol-2-yl)-3-(4H-1,2,4-triazol-3-yl)urea (7a): IR (KBr) νmax in cm-1: 3326 (N-H), 3081(Ar C-H), 1680 (O=C-N),1610 (C=N), 1472 (Ar C=C), 1214 (C-N), 2980(CH3); 1H NMR (DMSO-d6) δ: 2.37(s, 3H,CH3), 7.18-7.71 ( m, 3H, Ar-H), 12.00(s,1H,NH), 2.2 (s,1H,CH), 4.2(s,1H,NH), 4.2(s,1H,NH); MS m/z: 276[M+1]; Anal. Calcd. For C11H11N6O5: C, 48.17; H,3.67; N, 30.64%. Found: C, 48.10; H,3.57; N, 30.54%.
1-(6-Nitrobenzothiazol-2-yl)-3-(4H-1,2,4-triazol-3-yl)urea (7b): IR (KBr) νmax in cm-1: 3421(N-H), 1609 (O=C-N), 1476(Ar C=C), 1230(C-N),1343 (R-NO2), 762 (Ar-bend C-H); 1H NMR (DMSO-d6) δ:9.0(s,1H,NH), 2.6(s,1H,CH), 4.2(s, 1H,NH), 7.8-8.2(m,3H, Ar-H), 4.3(s,1H,NH); MS m/z: 305[M+2]; Anal. Calcd. For C10H7N7O3S: C,39.34; H, 2.31; N,32.12% Found: C,39.14; H, 2.21; N,32.22%
1-(6-Chlorobenzothiazol-2-yl)-3-(4H-1,2,4-triazol-3-yl)urea (7c): IR (KBr) νmax in cm-1: 3418(N-H.), 3092(Ar.C-H), 1608(O=C-N), 1479(Ar C=C), 1244(C-N), 760( R-Cl); 1H NMR (DMSO-d6)δ:7.55-8.20(m,3H,Ar), 6.0( d,2H,NH), 4.3(s,1H,NH), 2.6(s,1H,NH); MS m/z: 295[M+1]; Anal. Calcd. For C10H7N6OSCl: C, 40.75; H,2.39; N,28.52% Found: C, 40.55; H,2.38; N,28.51%
1-(6-Methoxybenzothiazol-2-yl)-3-(4H-1,2,4-triazol-3-yl)urea (7d): IR (KBr) νmax in cm-1: 3420(N-H), 3084(Ar C-H.), 1605(O=C-N), 1454(Ar C=C), 1314(C-N), 1297 (R-O-CH3): 1H NMR (DMSO-d6) δ: 7.06-8.12(m.3H,Ar), 3.73(s, 3H,CH3),6( s,2H,NH), 4.3(s,1H,NH), 2.6(s, 1H,CH); MS m/z:292[M+5]; Anal. Calcd. For C11H10N6O2S: C,45.51; H,3.47; N,28.95% Found: C,45.41; H,3.48; N,28.85%.
2.1.7. 1-(6-H-benzothiazol-2-yl)-3-(4H-1,2,4-triazol-3-yl)urea (7e): IR (KBr) νmax in cm-1: 3416(N-H.), 3085(Ar C-H.), 1610(O=C-N), 1475(Ar C=C), 1250 (C-N); 1H NMR (DMSO-d6) δ:7.55-8.23(m,3H, Ar), 6(s,1H,NH), 5.2 (s,1H,NH), 4.3( s,1H,NH), 2.6(s,1H,CH); MS m/z: 262 [M+2]; Anal. Calcd. For C10H8N6OS: C,46.15; H,3.10; N,32.29 %. Found: C,46.12; H,3.11; N,32.24 %.
1-(6-Sulfanilamidobenzothiazol-2-yl)-3-(4sH-1,2,4-triazol-3-yl)urea (7f): IR (KBr) νmax in cm-1: 3424(NH), 1608(O=C-N), 1468(Ar C=C), 1233(C-N), 762(Ar-bendC-H); 1HNMR (DMSO-d6) δ:8.22-8.55(m,3H,Ar.), 2.0(s,2H, NH2), 6( s,2H,NH), 4.3(s,1H,NH), 2.6(s,1H,CH); MS m/z: 308 [M+1]; Anal. Calcd. For C10H9N7O3S: C,35.39; H,2.36; N,28.89; %. Found: C,35.32; H,2.31; N,28.85%
Characterization data for (1-((3-(6-substituted-2-yl)ureido)methyl)cyclohexyl)acetic acid 8a-f (8a-f)
2-(1-((3-(6-Methylbenzothiazol-2-yl)ureido)methyl)cyclohexyl)acetic acid (8a): IR (KBr) νmax in cm-1: 3425(N-H), 1721(COOH), 1610(O=C-N), 1472(Ar C=C), 1298(C-N), 2983(ArC-H),2935(CH3)1HNMR(DMSO-d6)δ: 1.4(s,2H,CH2), 1.8-1.8( m,10H,Cyclohexane), 4.2(s,2H, CH2), 6.8(s,2H,NH), 2.37(s,3H,CH3), 7.6-7.8(m,3H,Ar-H), 11(s, 1H, COOH); MS m/z: 350 [M+1]; Anal. Calcd. For C17H23N3O3S: C, 59.81; H,6.41; N,11.63%. Found: C, 59.71; H,6.31; N,11.53%.
2-(1-((3-(6-Nitrobenzothiazol-2-yl)ureido)methyl)cyclohexyl)acetic acid (8b): IR (KBr) νmax in cm-1: 3420(N-H), 3088(Ar C-H.), 1717(COOH), 1610(O=C-N), 1561(R-NO2), 1476(Ar C=C), 1134(C-N); 1H NMR (DMSO-d6) δ:1.4(s,2H, CH2), 1.6-1.8(m,10H,Cyclohexane), 4.2(s,2H,CH2), 6.8(s,2H,NH), 7.6-7.8(m,3H,Ar-H), 10.5(s,1H, COOH); MS m/z: 393 [M+1]; Anal. Calcd. For C17H20N4O5S: C,52.03; H,5.14;N,14.28% Found:, 52.013; H,5.11;N,14.21%
2-(1-((3-(6-Chlorolbenzothiazol-2-yl)ureido)methyl)cyclohexyl)acetic acid (8c): IR (KBr) νmax in cm-1: 3418 (N-H), 3092(Ar C-H), 1610(O=C-N), 1608(C=N), 1436(Ar C=C), 1244(C-N), 781(R-Cl); 1H NMR (DMSO-d6)δ: 7.50-4.21 (t, 3H, Ar-H), 6.24( d,2H,NH), 2.14(s,2H,CH2),3.09(s,2H,CH2), 11.14( s,1H,OH), 1.00-1.70(d,2H, Cyclohexane), 1.34-1.37( d,2H, Cyclohexane), 1.42(d,2H, Cyclohexane), 1.34(d,2H, Cyclohexane), 1.56 (d,2H, Cyclohexane); MS m/z: 382 [M+1]; Anal. Calcd. For C17H20N3O3SCl: C, 53.47; H, 5.28; N, 11.00% Found: C, 53.44; H, 5.24; N, 10.95%.
2-(1-((3-(6-Methoxybenzothiazol-2-yl)ureido)methyl)cyclohexyl)acetic acid (8d): IR in cm-1[KBr] νmax: 3419 (N-H.), 3174(Ar C-H), 1605(O=C-N), 1714(COOH), 1454(C=C Ar.), 1297(C-N), 1119(R-O-CH3); 1H NMR (DMSO-d6)δ:7.05-8.15( t,3H,Ar.), 5.8(s,1H,NH), 6.5(s,1H,NH), 3.73 (s,3H,CH3), 2.15-3.08(d,4H,CH2),10.9(s,1H,OH), 1.06-1.56(m,10H, ,Cyclohexane); 377 [M+1]; Anal. Calcd. For C18H23N3O4S: C, 57.28; H, 6.14; N, 11.13%. Found: C, 57.18; H, 6.04; N, 11.03%.
2-(1-((3-(6-H-benzothiazol-2-yl)ureido)methyl)cyclohexyl)acetic acid (8e): IR in cm-1[KBr] νmax: 3440 (N-H), 3174(Ar C-H.), 1607(O=C-N), 1715 (COOH), 1455(C=C Ar.), 1284(C-N), 1H NMR (DMSO-d6) δ: 7.45-8.25(t,3H,Ar.), 7.55(S,H,1H), 5.8(s,1H,NH), 5.8(d,2H,NH),3.08(d,2H,CH2),2.15(d,2H,CH2),10.9(s,1H,OH),1.061.56(m,10H,Cyclohexane); MS m/z: 349 [M+2]; Anal. Calcd. For C17H21N3O3S: C, 58.77; H, 6.09; N, 12.09 Found: C, 58.57; H, 6.01; N, 12.01%
2-(1-((3-(6-Sulfanilamidobenzothiazol-2-yl)ureido)methyl)cyclohexyl)acetiacid (8f): IR in cm-1[KBr] νmax: 3320 (N-H), 3065(Ar.C-H), 1612(O=C-N), 1717(COOH), 1476(C=C Ar.), 1134(C-N); 1H NMR (DMSO-d6) δ:8.20-8.55( t,3H,Ar.),2.0( s,2H,NH2), 5.8(s,1H,NH), 6.0(d,2H,NH2), 3.73 (s,3H,CH3), 2.15(d,2H,CH2), 3.09( d,2H, CH2) 11.03(s,1H,OH), 1.05-1.55(m,10H, ,Cyclohexane); MS m/z: 427 [M+1]; Anal. Calcd. For C17H22N4O5S2: C, 47.87; H, 5.20; N, 13.14%. Found: C, 47.77; H, 5.14; N, 13.10%.
Biological Activity
Swiss albino mice of either sex weighing 20-25 g and Wister albino rat of either sex weighed 180-200 g were obtained from National institute biosciences, Pune . All animals were housed under normal ambient temperature conditions (25±20C) and 50±5 percent relative humidity. 12:12 hour light: dark cycle was maintained. All animals were permitted to have free access 24 hours prior to pharmacological studies to water and regular palletized laboratory animal diet. All the experimental procedures and protocols used in this study were reviewed and approved by the Institutional Animal Ethical Committee (IAEC) of Charak College of Pharmacy and Science, Pune, in accordance with the guidelines of the Committee for the Purpose of Animal Experiments Control and Supervision (CPCSEA), Government of India with Protocol No JSPM / CCOPR / PHARM/15/2012-2013.
CNS depressant activity by Actophotometer
All animals were randomly divided in to thirteen groups each containing 6 mice. All animal were weighed and numbered. Turn on the actophotometer and place the individual animal of each group in activity cage for 5 min. The basal activity score of animal was noted. Test compound at dose of 200 mg/kg orally was administered and after 55 min, the animal was again taken in actophotometer and the count was recorded. Similarly the activity was performed for all the remaining animals in the group and the Photoactometer count was recorded. The difference in basal activity before and after administration of drug was calculated. Similarly the activity for standard phenytoin and other compounds were recorded. [Table 2] Reduction in the motor activity indicates CNS depressant property of test compounds [17].
| Groups | Actophotometer readings for 5 min (Mean±SEM) | % CNS depressant Activity | |
|---|---|---|---|
| Before treatment | After 1hrs of administration | ||
| 7a | 310 | 173.66 ± 2.108** | 43.98 |
| 7b | 298 | 146.5 ± 1.310* | 50.83 |
| 7c | 315 | 171.66 ± 1.978** | 45.55 |
| 7d | 350 | 188.166 ± 2.880** | 46.24 |
| 7e | 305 | 137.66 ± 1.382 | 54.86 |
| 7f | 327 | 184.83 ± 1.579** | 43.47 |
| 8a | 323 | 177.5 ± 2.125** | 45.04 |
| 8b | 312 | 168.66 ± 0.663** | 45.94 |
| 8c | 295 | 135.5 ± 1.118 | 54.06 |
| 8d | 356 | 158 ± 1.238** | 55.17 |
| 8e | 343 | 208.5 ± 2.487** | 39.21 |
| 8f | 324 | 144.16 ± 1.302 | 55.50 |
| Phenytoin (STD)* | 295 | 137.66 ± 1.687 | 53.55 |
*STD: Standard
Evaluation of anticonvulsant activity using Maximum Electric Shock (MES) induced method by electroconvulsiometer
For the study, albino mice of either sex weighing 20-25 g are used. They were divided into fourteen groups of 6 mice each. The 0.1 percent sodium CMC solution is used as a test compound vehicle. The control group was injected with 1 ml (oral) of sodium CMC solution. As standard, Phenytoin 20 mg / kg (orally) is used. Test groups are handled separately with 200 mg / kg (orally) of 12 compounds each. After 60 min of test formulation administration, mice received 48mA current for 2s duration via electro convulsometer using ear electrodes. The animals were carefully examined for 2 minutes. The duration of tonic flexion and latency of onset of clonus have been reported. A complete abolition of the extension of hind limb tonic was considered as 100 percent protection [Table 3].The ability to prevent this feature is considered as an indication of anticonvulsant activity.
| Group | Onset of Action(Sec) Mean ± SEM | Total durations(Sec) Mean ± SEM | % Protection |
|---|---|---|---|
| 7a | 2.635 (± 0.80) | 30.1(± 2.73)** | 50% |
| 7b | 4.627 (± 1.98*) | 31.025(± 3.85)* | 83.33% |
| 7c | 2.035 (± 0.15) | 60.59(± 2.17) | 66.66 % |
| 7d | 1.455 (± 0.25) | 68.74(± 2.80) | 66.66 % |
| 7e | 2.49 (±0.89) | 77.153(± 3.07) | 100 % |
| 7f | 4.447 (± 1.16)* | 35.8(± 3.10)** | 66.66 % |
| 8a | 1.547(±0.23) | 65.91(± 0.69) | 66.66 % |
| 8b | 6.3725 (±1.86)** | 51.76(± 2.23) | 50 % |
| 8c | 1.165 (± 0.26) | 38.46(± 1.71)** | 100 % |
| 8d | 2.482 (± 0.14) | 65.27(± 3.01) | 33.33% |
| 8e | 1.815(± 0.34) | 47.695(± 2.41) | 66.66% |
| 8f | 1.92(± 0.24) | 65.71(± 2.46) | 50 % |
| Control | 0.57 ± 0.20 | 0.625 ± 0.03 | 0% |
| Phenytoin (STD)* | 4.36 ± 2.32 | 38.055 ± 2.71 | 100% |
*STD: Standard
Statistical analysis
Results are expressed as mean ± S.E.M. Statistical significance is tested using ANOVA Dunnet’s t-test. The difference is taken to be statistically significant at ** p < 0.01 and * p < 0.05 [18].
Molecular docking study
Protein preparation
Protein Data Bank (PDB; http:/ www.rcsb.org/pdb) was used to obtain the 3D crystal structure of GABA-AT enzyme with PDB ID: 1OHV [19] and hydrogens were added. Polar hydrogens should be present to validate the AutoDock groups, while non-polar hydrogens and the lone pair should be merged; Gasteiger partial charges should be allocated to each atom.
Ligand design
One of the most important determinants for effective docking is the structure of ligands, so pre-analysis of the structures of ligands is most important. Drugs such as ligand properties were confirmed by manually applying the Rule of Five of Lipinski and used for further studies. To draw the structure of the ligands Chem & Bio Draw 12.0 was used. In 2D, the ligands were cleaned and more energy reduced in 3D by the Chem & Bio 3D 12.0 documentation's MM2 parameters and force field. Initial ionization states were maintained and from 3D structures chirality’s were deter-mined. All the structures were written in mol2 file format and then modified into pdb format. Auto Dock requires that ligands for each atom give partial atomic charges and types of Auto Dock atoms; it also requires a description of the ligands' rotatable bonds. Auto Dock relies on the idea of a tree in which the 'root' is the rigid center of the molecule and the 'branches' extending from the root are flexible sections. This collection comprises, among others, of unified atoms, aromatic carbons in a cycle, aliphatic carbons, nitrogen bonded to hydrogen, polar hydrogen and oxygen bonded directly to hydrogen, each with partial charges. The pdbqt format was therefore used for ligands found by Auto Dock.
Auto Dock enables a completely versatile simulation, close to that of ligands, of particular portions of the receptor. In the current analysis, the binding site was selected on the basis of residues of amino acids involved in binding to a GABA-AT enzyme obtained from the ID 1OHV Protein Data Bank. The grid was then based around the area with amino acid residues (GLY136, SER137, GLN301, LYS329, ASN352, THR353) surrounding the active sites. In the docking process, a grid map of 68×42×66 points, a grid spacing of 0.375 A and a map of the ligand binding sites with centers x = 25.24, y = -16 and z = 25.25 were used. The Lamarckian Genetic Algorithm (LGA) was used to find the conformers with the lowest binding energy based on an optimization algorithm. Finally, the docking task was performed using Easy Dock-Vina v2.0 (Auto Dock vina GUI. Easy Dock Vina is a software for multiple Auto Dock Vina Receptor-Ligand docking. It uses Auto Dock Vina for docking, MGL tools and open babel for molecular preparation are also used. The results of molecular docking studies were obtained in output files in the form of calculated free energy by Pymol and Discovery Studio Visualizer, which examined hydrogen, hydrophobic, and van der Waals contacts, were used for visualization and analysis of docking results.
In silico ADME prediction
For the prediction of ADME properties, a computational study of synthesized compounds 7a-f and 8a-f was carried out. partition coefficient logarithm (miLog P), molecular weight (MW), Molecular volume (MV), hydrogen bond donor number (n-OHNH), hydrogen bond acceptor number (n-ON), number of rotatable bonds (n-ROTB), topological polar surface area (TPSA), and Lipinski's rule of five were measured using the Molinspiration online property calculation toolkit. Absorption (% ABS) was determined by applying formula:
% ABS = 109 - (0.345 × TPSA) [20].
Result and Discussions
Chemistry
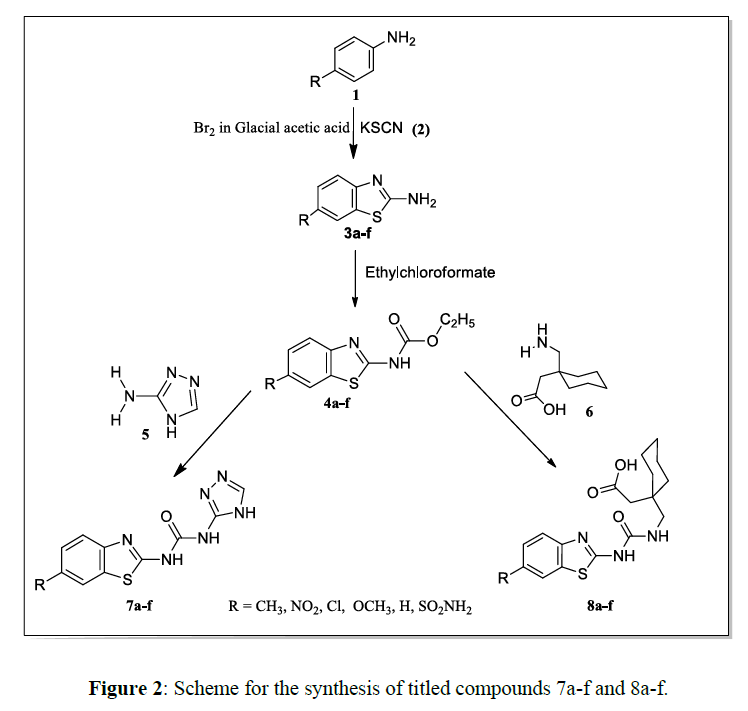
Synthesis of titled compounds 7a-f and 8a-f has been carried out as depicted in the scheme 1. The starting substituted 2-amino Benzothiazole 3a-f were synthesized by reacting substituted aniline (1) with potassium thiocyanate(2) in bromine glacial acetic acid [21]. The compound 3a-f were stirred with ethyl chloroformate in the presence of dichloromethane and triethylamine in ice cold condition for 3 hours to afford 4a-f [22]. Triazole derivatives 7a-f were obtained by refluxing compounds 4a-f with 3-amino-1,2,4-traizole (5) in methanol for 4 h. Similarly gabapentin derivatives 8a-f were obtained by refluxing compounds 4a-f with gabapentin(6) independently. All synthesized compounds compound were characterized by analytical and spectral data (Table 1).
The nucleophilic attack of p- substituted aniline on potassium thiocyanate which afforded an intermediate phenylthiourea which on cyclisation reaction in presence of bromine yielded compounds 3a-f. Synthesis of compound 4a-f involve chloroformylation of primary amine of 6-substituted-2-amino Benzothiazole by using ethyl chloroformate in presence of triethylamineas a base. The triazole derivatives 7a-f involve esteraminolysis reaction with neucleophilic attack of primary amino group of 3- amino-1,2,4-triazole and gabapentin independently on carbonyl carbon of 4a-f which will be converted into final target derivatives 7a-f and 8a-f. [23-24].
Biological activity
CNS depressant activity
The preliminary evaluation of synthesized compounds, 1-(6- substituted Benzothiazole -2-yl)-3-(4H-1,2,4-triazole-3-yl) urea 7a-f and 2-(1-((3(6-substituted Benzothiazole-2-yl) ureido) methyl) cyclohexyl) acetic acid 8a-f were carried out for CNS depressant activity using actophotometer. The difference in basal activity before and after administration of drug were calculated and compared with standard phenytoin. Reduction in motor activity indicates CNS depressant property. The test Compounds 7a, 7b, 7c, 7d, 7f, 8a, 8b, 8d and 8e were exhibited significant activity as compared to phenytoin in the range of 50.00-55.50 (Table 2).
Anticonvulsant activity using Maximum Electric Shock (MES) method
Anticonvulsant activity was evaluated using MES induced method by electroconvulsiometer Mice were received current of 48mA for 2s duration through electroconvulsiometer using ear electrodes after 60 min of administration of test formulation. Phenytoin was used as standard. The compound 7a, 7f and 8b exhibited significant activity in mice at does 200mg/kg. The standard phenytoin required 4.36 sec to inhibit the seizures in mice, while 7a and 7f were showed activity at 4.62 and 4.44 sec respectively. Compound 8b inhibit seizures at much better time i.e. 6.37 sec as compared to standard. The compounds possessing electron donating group substitutions on Benzothiazole ring were found to exhibited significant activity compared to other compounds (Table 3).
Oral acute toxicities study
To assess the lethal dose of the test substances, an oral acute toxicity analysis was performed. Animal groups of non-pregnant women were dosed with fixed doses of 5, 50, 300 and 2000 mg / kg in a stepwise process. This procedure continues until a dose is identified which causes apparent toxicity or no more than one death. The suspension of test compounds was administered orally in sodium CMC. A dose of 5 mg / kg was administered to the first test sample. For 24 hours, the animals were observed. Similarly other groups of animals were administered the test compounds at a dose of 50, 300 and 2000 mg/kg and observations were made on subsequent day after 24 h. of administration of dose for mortality. The lethal dose of compound 6a was found 2000mg/kg. Hence the 1/10th of the lethal dose i.e. 200mg/kg was selected as dose of test compound for the study.
Molecular docking studies
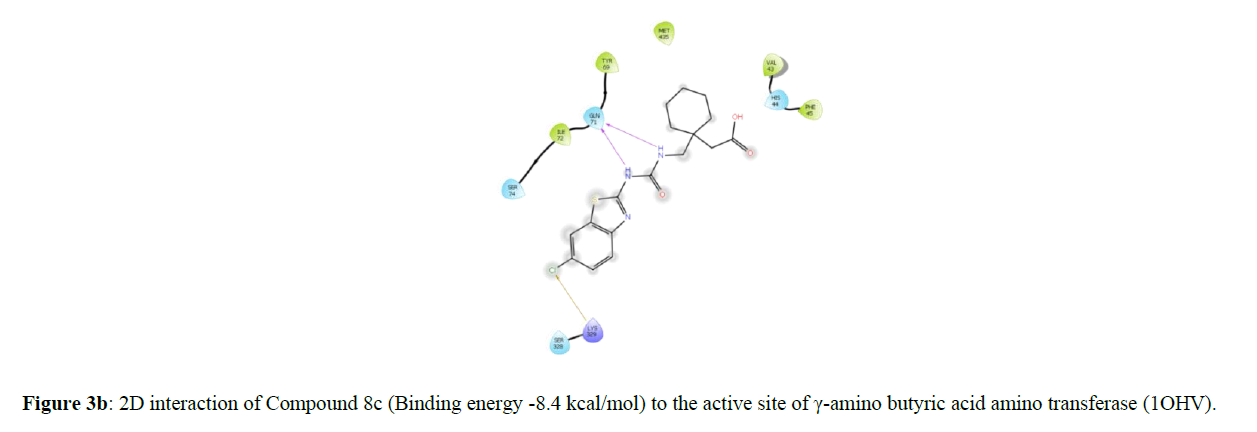
Molecular docking studies have been conducted on the γ-amino butyric acid amino transferase [GABA-AT] enzyme to determine the interactions of designed target molecules with receptors. GABA-AT is a valid target for AEDs. Its selective inhibition raises concentration of GABA in brain. GABA is inhibitory neurotransmitter. Hence GABA-AT was selected as target for anticonvulsant activity. The docking study was carried out on AutoDock 1.5.6 to predict potential binding interactions using 1OHV PDB. The grid was based around the area surrounding the active sites, including amino acid residues (GLY136, SER137, GLN301, LYS329, ASN352, and THR353). The results were compared with standard phenytoin on same receptor. All 12 derivatives were exhibited docking score in range of -7.5 to -8.4 (Table 4) and standard phenytoin dock score is -8.9. Further review of the findings revealed that the chlorosubstituted derivative (8c) showed the highest receptor affinity interacting with amino acid residue ARG192, LYS203, GLU270,TYR348, ILE426, GLY438 and ARG445 (Figure 3a-3b).In comparison to standard drug Phenytoin withinteracting amino acids TYR69, ILE72, ILE105, ARG192, LYS203, HIS206, GLU270,TYR348, PHE351, GLY438, GLY440 and ARG445 of 1OHV PDB [Figure 4a-4b].
| Code | R | Docking score | Log p |
|---|---|---|---|
| 7a | CH3 | -7.5 | 2.23 |
| 7b | NO2 | -8.1 | 1.55 |
| 7c | Cl | -7.5 | 2.75 |
| 7d | OCH3 | -7.3 | 1.62 |
| 7e | H | -8.2 | 1.75 |
| 7f | SO2NH2 | -7.7 | 0.49 |
| 8a | CH3 | -8.1 | 4.06 |
| 8b | NO2 | -8.3 | 3.38 |
| 8c | Cl | -8.4 | 4.13 |
| 8d | OCH3 | -7.9 | 3.45 |
| 8e | H | -8.2 | 3.58 |
| 8f | SO2NH2 | -8.3 | 2.32 |
| Standard | Phenytoin | -8.9 | 2.14 |
In silico ADME prediction
The in silico ADME prediction of the titled compounds 7a-f and 8a-f was performed using Molinspiration online property calculation toolkit (http://www.molinspiration.com/cgi-bin/properties 2014), and the results are provided in Table 5. All synthesized antipyrine derivatives have a good % ABS ranging from 71.03-78.51%. Also, none of the synthesized compounds violated the Lipinski rule of five, thus showing good drug-like properties. A molecule likely to be developed as an orally active drug candidate should not violate more than one of the following four criteria: molecular weight ≤ 500, miLogP (octanol-water partition coefficient) ≤ 5, number of hydrogen bond donors ≤ 5, and number of hydrogen bond acceptors ≤ 10. All the compounds 4a–I follow the criteria for orally active drug, and therefore, these compounds may have good potential as oral agents for subsequent development.
| Compound | %ABS | TPSA | MV | n-ROTB | miLogP | MW | n-ON acceptors | n-OHNH donors | Lipinski's violations |
|---|---|---|---|---|---|---|---|---|---|
| 7a | 76.02 | 95.59 | 223.02 | 2 | 1.9 | 274.31 | 7 | 3 | 0 |
| 7b | 60.21 | 141.42 | 229.79 | 3 | 1.41 | 305.28 | 10 | 3 | 0 |
| 7c | 76.02 | 95.59 | 220.00 | 2 | 2.13 | 294.73 | 7 | 3 | 0 |
| 7d | 72.83 | 104.83 | 232.01 | 3 | 1.51 | 290.31 | 8 | 3 | 0 |
| 7e | 76.02 | 95.59 | 206.46 | 2 | 1.48 | 260.28 | 7 | 3 | 0 |
| 7f | 57.96 | 147.92 | 252.41 | 4 | 0.83 | 339.36 | 10 | 5 | 0 |
| 8a | 77.49 | 91.32 | 325.22 | 5 | 3.93 | 361.47 | 6 | 3 | 0 |
| 8b | 61.68 | 137.14 | 331.99 | 6 | 3.44 | 392.44 | 9 | 3 | 0 |
| 8c | 77.49 | 91.32 | 322.19 | 5 | 4.16 | 381.88 | 6 | 3 | 0 |
| 8d | 74.31 | 100.55 | 334.2 | 6 | 3.54 | 377.47 | 7 | 3 | 0 |
| 8e | 77.49 | 91.32 | 308.65 | 5 | 3.51 | 347.44 | 6 | 3 | 0 |
| 8f | 56.73 | 151.48 | 351.38 | 6 | 2.18 | 426.52 | 9 | 5 | 0 |
Absorption (% ABS), molecular volume (MV), molecular weight (MW), logarithm of partition coefficient (miLog P), number of hydrogen bond acceptors (n-ON), number of hydrogen bond donors (n-OHNH), topological polar surface area (TPSA), number of rotatable bonds (n-ROTB)
Conclusion
A series of 1-((-6-substituted-2-yl)-3-(4H-1,2,4 triazole-3-yl)urea 7a-f and (1-((3-(6-substituted-2-yl)ureido)methyl)cyclohexyl)acetic acid 8a-f were designed by molecular docking study and synthesized using appropriate synthetic route. The structures of the synthesized compounds were confirmed using different spectroscopic techniques. All the compounds exhibited docking score in the range of -7.5 to -8.4.Compounds 7b, 7e and 8c were exhibited significant anticonvulsant and CNS depressant activity at a dose 200 mg/kg. The results gained can be used for future development of more active agents.
Acknowledgement
Authors are grateful to the Prof. T. J. Sawant, Founder secretary, Charak College of Pharmacy and Research, Wagholi, Pune, India for providing necessary facilities for the research work.PadmashreeFatma Rafiq Zakaria, Chairman of MAET and Principal, Y. B. Chavan College of Pharmacy for encouragement.
References
- Cloyd J, Hauser W, Towne A et al., EpilepRes. 2006, 68: p. 39–48.
- Elger CE and Schmidt D. Epilepsy Behav. 2008, 12 (4): p. 501–539.
- Fisher R. Comprehensive Epilepsy Center. 2010, 2.
- Hassan MZ, Khan SA and Amir M. Eur. J. Med. Chem. 2012, 58: p. 206–213.
- Khokra S, Aarora K, Mehta H et al., Int J Pharm Sci Res. 2011, 26: p. 1356–1377.
- Kulkarni S. Vallabh Prakashan. 2005.
- Kumbhare R, Kosurkar U, Ramaiah M et al., Bio Med Chem Lett. 2012, 22: p. 5424–5427.
- Malik J, Manvi F, Nanjwade B et al., Der Pharm Lett. 2010, 2: p. 347–359.
- Moreno DH, Villalobos MR, Ortiz AR et al., Bio Med Chem Lett. 2008, 18: p. 2871–2877.
- Schachter SC. Epilepsy Res. 2002, 50: p. 67–70.
- Shashank D, Vishawanth T, Pasha M et al., Inter Jour Chem J Technol Res. 2009, 14: p. 1224–1231.
- Shaw G, Sreenivasa G and Jayachandran E. Orient J Chem. 2008, 242: p. 475–484.
- Shinnar S and Berg AT. Epilepsia. 1996, 37(8): p. 701–708.
- Siddiqui N, Rana A, Khan SA et al., Bioorg Med Chem Lett. 2007, 17(15): p. 4178–4182.
- Singh MK, Tilak R, Nath G et al., Eur J Med Chem. 2013, 63: p. 635–644.
- Temkin NR. Epilepsia. 2001, 42(4): p. 515–524.
- Ugale VG, Patel HM, Wadodkar SG et al., Eur J Med Chem. 2012, 53: p. 107–113.
- Vogel H. Springer: Berlin, 2002.
- Williams D and Emke T. Foye’s Principles of Medicinal Chemistry. 2005, 384.
- Yoshida M, Hayakawa I, Hayashi N et al., Bio Med Chem Lett. 2005, 15: p. 3328–3332.
- Zhao YH, Abraham MH, Le J et al., Pharm Res. 2002, 19(10): p. 1446–1457.
- Tanino T, Ogiso T, Iwaki M et al., Jour Pharm. 1998, 163: p. 91–102.
- Smith M and March J. Wiley Interscience. 2001.
- Ghosh S. Advanced General Organic Chemistry. 2007, p. 596-97.