Review - Der Pharma Chemica ( 2024) Volume 16, Issue 5
Current Trends in Breast Cancer Treatments
Kalyani R. Thombre, Krishna R. Gupta* and Milind J. UmekarKrishna R. Gupta, Department of Pharmaceutical Chemistry, Smt. Kishoritai Bhoyar College of Pharmacy, New Kamptee, Nagpur, India, Email: krg1903@gmail.com
Received: 02-Mar-2024, Manuscript No. DPC-24-148557; Editor assigned: 06-Mar-2024, Pre QC No. DPC-24-148557 (PQ); Reviewed: 20-Mar-2024, QC No. DPC-24-148557; Revised: 01-Oct-2024, Manuscript No. DPC-24-148557 (R); Published: 29-Oct-2024, DOI: 10.4172/0975-413X.16.5.458-468
Abstract
Worldwide, Breast Cancer (BC) remains the most common cancer type accounting for approximately 2.3 million new cases and 685, 000 deaths in 2020. Despite advances in early detection and treatment, breast cancer continues to pose significant challenges due to different molecular subtypes posing different therapeutic challenges. Genetic and hereditary predispositions are among the numerous risk factors linked to the development of breast cancer. The spectrum of breast cancers is very wide. Early-stage breast cancer is thought to be curable and the mainstay of treatment for it is local-regional therapy (radiation and surgery), with systemic therapy administered either before or after surgery as needed. The conventional therapy for early-stage BC is mastectomy alone or breast-conserving surgery coupled with radiation and lymph node, ER, PR and HER-2 status. Breast cancer therapy has evolved from a surgical method to a more comprehensive strategy. Preoperative or neoadjuvant therapy is now necessary for most cases of early-stage breast cancer and may involve immune checkpoint inhibitors. Endocrine therapy and chemotherapy are the most common therapies for persons with hormone-positive (ER+ and HER2+) breast cancer making them simpler to treat. Immunotherapy is developing as an important part of breast cancer, treatment. Despite initial disappointments immunomodulation and cancer vaccines have shown clinical benefits. Gene therapy introduces genetic material into target cells via a vector, followed by gene correction, addition or suppression. The present review explores current trends in breast cancer treatments, including surgery, endocrine therapy chemotherapy, radiotherapy, immunotherapy and gene therapy. Finding new treatment targets, refining combination medicines and comprehending the function of tumor evolution should be the top priorities for future research. Improving patient outcomes will require a focus on combining genetic and proteomic data to enhance precision medicine and a study of the social and psychological aspects affecting treatment adherence. Through this review, we propose to highlight the critical need for further study and a multidisciplinary strategy to understand the complexity of breast cancer and eventually increase patient survival rates and quality of life.
Keywords
Breast cancer; Surgery; Endocrine therapy; Immunotherapy; Gene therapy; Radiotherapy
Introduction
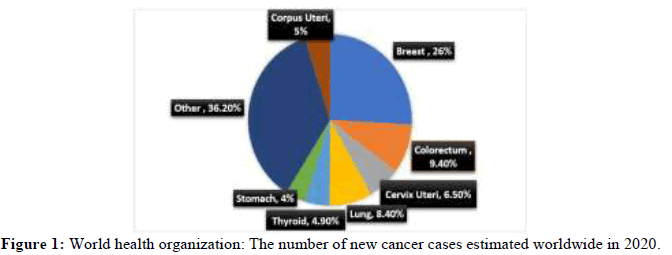
Cancer is now the leading cause of death worldwide, estimated 19.3 million new cases in 2020, killing more than 10 million people or about one in six. The most common cancers are breast, lung, colon, rectum and prostate cancer although many significant advances have been made recently (Figure 1).
Breast cancer, the most common disease in women worldwide, is a major public health issue that requires increasing attention and collaborative research efforts. Breast cancer is a diverse illness with various biological and clinical features. Female breast cancer is now the most often diagnosed cancer worldwide, surpassing lung cancer. In 2020, the projected number of new breast cancer cases in the world was 2.3 million accounting for 25-30% of all cancers. According to GLOBOCAN 2020, the global breast cancer incidence and mortality in 2020 were 34,65,951 new cases and 11,21,413 deaths. Globally female breast cancer death rates were much higher in transitioning vs. transitioned nations (15.0 vs. 12.8 per 100,000). While women in transitional nations have incidence rates that are significantly greater than those in transitioning countries (54.1 vs. 30.8 per 100,000, respectively), their mortality rates are significantly lower (11.3 vs. 15.3 per 100,000, respectively). The greater prevalence of various reproductive and lifestyle risk factors, such as early menarche age, late menopause age, advanced age at first birth, fewer children, less breastfeeding, hormone replacement therapy, oral contraceptive use, alcohol consumption, excess body weight and physical inactivity, is reflected in the higher incidence rates in transitioned compared to transitioning countries [1].
Problems and knowledge gaps in breast cancer therapies
An equimolar mixture of substituted tryptophol and 1 3-dicarbonyl compound was allowed to stir at 0°C in IPA: Toluene solvent mixture. Catalytic Global breast cancer research faces significant obstacles that point to serious inequities. According to recent data from the World Health Organization (WHO), less than half of nations have palliative care plans 40% report significant management and treatment access restrictions and 62% report screening programs. These statistics are although 70% of countries have established cancer guidelines. Breast cancer is a multifactorial disorder and various risk factors include reproductive and hormonal factors (e.g., early menarche, late menopause, advanced age at first birth, fewer children, less breastfeeding, menopausal hormone therapy, oral contraceptives). Radiation exposure, lifestyle factors (e.g., obesity, physical inactivity, alcohol consumption, diet, smoking, dietary habits), family history, disease condition, genetic susceptibility, including mutations in high-penetrance genes including BRCA1/2, PALB2, ATM, CHEK2, RAD51C, BARD1 and TP53, can contribute to breast cancer. The changing patterns and causes influencing breast cancer prevalence highlight the importance of further study into the disease. Lifestyle changes, environmental exposures and demographic shifts all contribute to the rising incidence of breast cancer.
The extensively heterogeneous nature of breast cancer, as evidenced by its numerous molecular subtypes, poses therapy challenges; thus, it is necessary to distinguish between the various molecular and prognostic characteristics of these subtypes. The major molecular markers used to differentiate breast cancer subtypes are the presence or absence of the Estrogen Receptor (ER), Progesterone Receptor (PR) and Human Epidermal growth factor 2 (HER2) receptor proteins. Breast Cancer (BC) is a diverse disease classified into subgroups based on histological and molecular characteristics i.e., luminal A (ER+PR+HER2-) luminal B (ER+PR+HER2+) normal like HER2+ and TNBC (ER-PR-HER2-) [11]. There are currently few reliable biomarkers for predicting a patient's response to a particular therapy. Particularly in the context of immunotherapy and targeted treatments, finding and confirming novel biomarkers may help inform treatment choices, track the effectiveness of prescribed medications and reduce needless toxicity. Despite the development of new drugs, many patients develop resistance to therapies, such as endocrine therapy, targeted treatments and chemotherapy. The underlying mechanisms of primary and acquired resistance, including genetic mutations, epigenetic alterations and the role of the tumor microenvironment, remain inadequately understood [2].
Treatment response and breast cancer progression are significantly influenced by the Tumor Microenvironment (TME). Nevertheless, little is known about how cancer cells, immune cells and the extracellular matrix interact with the Tumor Microenvironment (TME). Further investigation is required to comprehend how the TME impacts treatment results and to pinpoint possible therapeutic targets within it. Diverse patient populations, such as older adults, members of racial and ethnic minorities, and those with comorbidities, are frequently absent from current clinical studies. This restricts the data' generalizability and could ignore differences in side effects and treatment response among other demographic groups. We are still in the early stages of personalizing breast cancer therapy through the integration of AI, ML, and sophisticated genomics in clinical settings. More studies are needed to evaluate these technologies' clinical value, accuracy and cost-effectiveness. It is clear that there are many stakeholders are involved in this complicated issue, and there are many factors to take into account. Putting the most significant first, we could contend that late-stage diagnoses, lack of timely and suitable diagnostic and treatment methods and access to healthcare. Table 1 shows different breast cancer subtypes. Therefore, we must face these challenges head on and obtain a deeper understanding of the disease's biological complexity. Despite advancements in oncology, breast cancer remains a worldwide health concern that requires additional research and innovative treatments [3].
| Breast cancer sub types | Molecular features | Incidence and prognostic features | |||
|---|---|---|---|---|---|
| ER | PR | HER2 | Ki-67 index | ||
| Luminal A | + | + | - | Low |
|
| Luminal B | + | + or - | - | High |
|
| + | + or - | + | Any | ||
| HER2-amplified | - | - | + | Any |
|
| Triple negative | - | - | - | Any |
|
| Note: ER: Estrogen Receptor; PR; Progesteron Receptor; HER2: Human Epithelial Growth Factor Receptor 2; Ki67: Antigen Kiel 67. | |||||
Table 1: Breast cancer Sub types: Incidence and prognosis.
Literature Review
This review aims to summarize the current state of the art and debates surrounding surgery, chemotherapy radiation therapy, endocrine therapy, immunotherapy, gene therapy and other cutting edge therapies for breast cancer. To treat breast cancer, a multidisciplinary team must collaborate on treatment plans that involve surgery, chemotherapy Radiotherapy (RT), endocrine therapy, targeted therapy and immunotherapy.
Breast cancer therapy options
Breast cancer screening guidelines should be based on risk stratification. Women are divided into two categories: Average risk and higher risk. The best method of lowering the risk of breast cancer is a bilateral mastectomy, which is advised for women who are significantly more vulnerable. Minimally invasive surgery is the standard treatment for non-metastatic breast cancer; however, prior systemic chemotherapy can reduce the volume of the tumor in the breast, sparing the breast and reducing the need for Axillary Lymph Node Dissection (ALND). Surgery is reserved for palliative care in a small proportion of metastatic patients and systemic therapy remains the preferred course of action for metastatic breast cancer.
Cancer immunotherapy is one of the most important developments in oncology in recent years. Breast Cancer (BC), historically thought to be low immunogenic, was not initially thoroughly studied for immunotherapy susceptibility. Clinical trials assessing various immune therapeutic approaches for BC patients have been developed due to recent advancements with Immune Checkpoint Inhibitors (ICI) in other cancers and mounting evidence of the immune system's role in cancer behavior.
Additional treatments for patients with metastatic and non-metastatic breast cancer are made possible by developments in endocrine therapy, chemotherapy, and radiotherapy. Promising outcomes have been observed in some novel therapies under investigation, including gene therapy (viral and non-viral), immunotherapies that involved cytokine therapy, monoclonal antibodies, vaccinesm, and adoptive cell therapy [4].
Selection of breast cancer therapy
For breast cancer in stages I to III, surgery and radiation therapy are the standard course of treatment. Chemotherapy or other pharmacological therapies are frequently used either before (neoadjuvant) or after (adjuvant) surgery. Treatments for breast cancer have a major impact on patient outcomes and survival rates. The therapies chosen depend on the kind and stage of the tumor and their efficacy is contingent upon the patient adhering to the prescribed course of action. Various treatment options for breast cancer treatment are summarized in Table 2 [5].
| Treatment option | About | Route of administration | Unique feature | Common side effects |
|---|---|---|---|---|
| Surgery | Removal of cancer from breast by operative procedure | NA | Performed alone or prior to or after chemotherapy | Hematoma, Seroma, pain, Lymphedema, infection and cosmetic issues |
| Chemotherapy | Directly killing the cells using drugs | Oral or intravenously | Drugs can slow cancer growth or harm healthy cells | Fatigue, hair loss, bruising or bleeding, infection, nausea, vomiting, appetite changes |
| Radiation | Use of high energy beams to damage cancer cells | Using Machine | Targeted destruction of cancer cells in breast left after surgery | Change in skin color, itching, soreness and possibly peeling |
| Hormone Therapy | Medication for hormone dependent breast cancer | Oral or injection in skin | Not allowing the hormones to nourish the breast cancer cell growth | Hot flashes, vaginal dryness, night sweat, bone pain |
| Biologic targeted therapy | Altering the behaviour of cancer cell | Intravenously or oral | Interferes with specific molecules in tumour growth or progression | Heart impairment, diarrhoea, shortness of breath |
| Immunotherapy | Improving immune system to fight against cancer cell | Intravenously | It works to boost persons own immune system to kill cancer cell | Flu like symptoms, rash Fatigue |
Table 2: Breast cancer treatments.
Early breast cancer treatment: Local and regional
Surgery: For many years, surgery has been used to treat breast cancer. Over the past few decades, there has been a significant evolution in the surgical treatment of breast cancer, with advancements made to minimize the long-term cosmetic and functional side effects of local therapy. Many experiments have moved from drastic methods to less drastic surgeries. Latest developments in breast cancer surgery:
Breast-Conserving Surgery (BCS): Breast-conserving surgery is referred to by several names, such as lumpectomy and quadrantectomy. Radiation therapy combined with Breast-Conserving Surgery (BCS) is now the accepted treatment for low-grade breast cancer. Early invasive breast cancer can be successfully managed locally with either Breast-Conserving Surgery (BCS) or mastectomy with or without immediate reconstruction. In all cases of early-stage breast cancer detection, it is the safest and most recommended treatment approach. The distant metastasis recurrence rates and distant metastasis rates have decreased in recent decades due to the widespread use of systematic treatments. For Estrogen Receptor (ER) positive and human epidermal growth factor receptor-2 (HER-2) positive breast cancer, the 10-year distant metastasis recurrence of BCS was 2%-3% and for Triple-Negative Breast Cancer (TNBC), it was 5%. The three most well-known local treatments for breast cancer surgery are:
• Oncoplastic surgery: Combining the best practices of cosmetic surgery with breast surgical oncology, oncoplastic surgery is a
developing area of breast surgery. It enables the surgeon the capacity to remove a significant portion of the breast during an
oncologic excision without sacrificing or perhaps even enhancing its cosmetic attractiveness.
• Intraoperative Radiation Therapy (IORT): it is a relatively recent technique intended for replacing External Beam Radiation
Treatment (EBRT) of the entire female breast who are recipients of breast-conserving therapy. It reduces the need for postoperative
radiation therapy and shortens the duration of treatment by delivering a single, specific dose of radiation erratically to the tumor bed
during surgery.
• Axillary Lymph Node Dissection (ALNDs): The state of the Axillary Lymph Nodes (ALNs) at diagnosis and neoadjuvant systemic
therapy determine how the ALNs are managed. In patients with clinically demonstrated axillary involvement at initial diagnosis,
ALND is still the standard practice. The management of axillary lymph nodes in patients with Clinically Node-Negative (cN0) breast
cancer is controversial. In the era of modern systemic treatments, there appeared to be similar survival and recurrence outcomes
between ALND and Sentinel Lymph Node (SLN) biopsy [6].
Minimally invasive surgery
Laparoscopic and robotic-assisted techniques: When performing minimally invasive procedures in the abdomen or pelvis with the help of a camera, such as in a laparoscopy, instruments are inserted through a relatively small incision. Catheters are frequently used in minimally invasive procedures carried out under image guidance in interventional radiology. Over time, the transition from open to minimally invasive procedures finally resulted in the application of robotic technologies to either support or replace patient-side surgery entirely with a distinct panel. For instance, angioplasty involves inserting a balloon into the narrowed or obstructed portion of the blood vessel using a catheter and then inflating the balloon to repair the vessel. The surgeon gains direct access to the surgical site when performing open surgery. Medical image analysis and visualization research has increased significantly as a result of the realization that minimally invasive and interventional procedures are best served by meticulous preoperative planning and guidance. Compared to traditional open surgery, allows for fewer incisions, less blood loss, shorter stays in the hospital and quicker recovery periods. Despite the positive surgical outcomes associated with robotic surgery some circumstances such as financial viability or spatial limitations limit its application.
Mastectomy: A mastectomy involves the complete removal of breast tissue. Recent years have seen an increase in the number of preventive mastectomies performed; this is partially due to an extreme underestimation of the risk of developing contralateral breast cancer. Contralateral preventative mastectomy is frequently most beneficial to patients who have an increased lifetime chance of developing contralateral breast cancer. This group includes patients with a robust family history, BRCA-positive individuals and any young patient with biologically aggressive breast disease. The most effective method of lowering the risk of breast cancer is a bilateral mastectomy, which is advised for women who are at extremely high risk (e.g., with radiation therapy to the breast before age 30 or a high-risk gene mutation for breast cancer). The terms "minimum effective treatment" and "conservative mastectomy" refer to a group of mastectomy procedures that includes skin-sparing and NSM. This group of procedures combines oncologic plastic surgery with tumor excision to create a skin flap that can be immediately rebuilt. Superior esthetical results are achieved while maintaining oncologic safety by preserving the nipple and areola complex. The two most well-known local treatments for breast cancer surgery are Breast-Conserving Surgery (BCS) and mastectomy with or without rapid reconstruction. The goal of these advancements in breast cancer surgery is to reduce the psychological and physical effects of therapy to enhance both oncologic results and patient satisfaction. Surgery is often a low-risk procedure for breast cancer patients. However, both lumpectomy and/or mastectomy might result in a variety of problems. Positive margins following a lumpectomy may need re-excision or mastectomy. Surgery is also necessary in the treatment of local-regional recurrent breast cancer. Salvage mastectomy with ALND can offer 85%-95% loco-regional control in this kind of cancer, while complete mastectomy is still the usual treatment for recurring patients who have undergone BCS. Patients who sustained chest-wall recurrence after the first mastectomy were more likely to develop metastases than those who were first treated with BCS. As a result, the widely prescribed therapy for patients first treated with mastectomy is wide excision of the reoccurring lesions whenever possible [7].
The problem with surgical treatment seems to be that patients' concerns about breast surgery varied and shared decision-making was not always used. Due to behavioral and cognitive biases, there were differences in information exchange behaviors, value clarification, use of decision assistance and shared decision making.
Radiotherapy
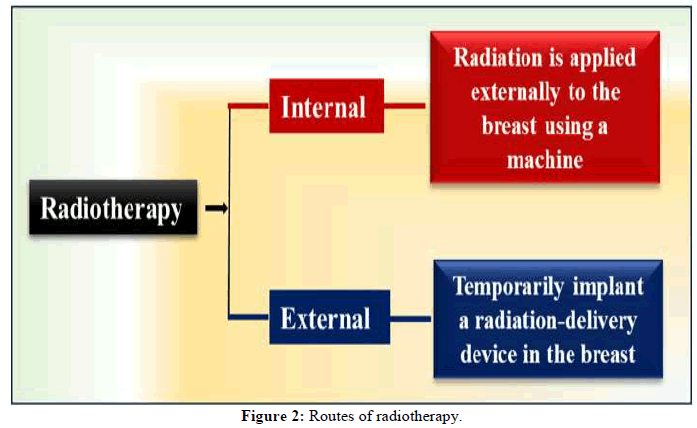
High-energy X-rays protons or other particles are used in radiation treatment for breast cancer to destroy cancer cells. Radiation therapy has a greater effect on rapidly developing cells than on normal cells, such as cancer cells. The X-rays or particles are painless and invisible. Postoperative radiotherapy is advised for individuals undergoing BCS or mastectomy (with risk factors). Breast cancer radiation treatment can be administered by internal and external routes as shown in Figure 2.
After BCS, Whole Breast Irradiation (WBI) is a practical alternative for adjuvant radiotherapy. Compared to WBI, hypo-fractionated WBI seems to have similar local recurrence survival rates and toxicity profiles. Breast cancer can be treated with radiation treatment in every stage of the disease. After surgery, radiation treatment is a useful tool for lowering the chance of breast cancer returning. Furthermore, it is frequently used to relieve the symptoms of metastatic breast cancer, a kind of cancer that has spread to other regions of the body. The amount of affected Axillary Lymph Nodes (ALNs) determines whether or not to irradiate patients undergoing mastectomy. Patients with four or more positive ALNs are often treated with Postmastectomy Radiation Treatment (PMRT); however, it is uncertain whether PMRT should be given to patients who have one to three implicated ALNs. Radiation to the chest wall and infra-/supraclavicular areas is effective for individuals with positive regional lymph nodes. In trials reported in the literature, all treated breast cancer patients' prospectively recorded treatment data showed a high level of adherence to pre-specified treatment planning limitations. This implies that more stringent dose restrictions can be used and are advised for upcoming whole breast radiotherapy planning for organs at risk and high dose breast volumes [8].
Discussion
Early breast cancer: Systemic treatment
Endocrine therapy: For female patients with hormone receptor-positive early-stage breast cancer, endocrine therapy continues to be the cornerstone of adjuvant treatment. Luminal A and B tumors are generally estrogen-dependent. Luminal breast cancer can be successfully treated with approaches that decrease estrogen receptor function. Endocrine therapy is a highly successful treatment option for ER or PRpositive breast cancer, which works by inhibiting the effects of hormones or decreasing hormone levels. Classical endocrine therapies modify the estrogen action by inhibiting the ER (selective ER modulators, SERMs) or aiming to diminish estrogen levels.
Recently available medications include Tamoxifen, a pioneering SERM, that inhibits estrogen activity by binding to the ER in breast tumors. Tamoxifen has been widely utilized in clinical practice for the treatment of breast cancer for the last 30 years and it is now accessible to minimize the risk of breast cancer in high-risk women. Aromatase inhibitors (letrozole, anastrozole and exemestane), are a class of medications that function by inhibiting the enzyme aromatase, which converts androgens to estrogen leading to estrogen reduction. Fulvestrant is a selective ER degrader. It is a first-generation SERD authorized by the FDA in 2007 for the treatment of metastatic luminal breast cancer in postmenopausal individuals following progression on previous ET with AI or tamoxifen. Luteinizing hormone-releasing hormone analogs (goserelin and leuprolide), inhibit hormone generation from the ovary.
These treatments are frequently quite effective; however, the tumor evolves with time and develops resistance in a variety of ways. Overcoming endocrine resistance is a significant hurdle while treating ER-positive breast cancer. Recurrences can happen five to twenty years after surgery, depending on the histological grade, nodal status and original tumor. Recurrent breast cancer has lost its requirement for estrogen, demanding unique therapy tailored to the newly discovered molecular aspects of the improving disease. Patients with a history of advanced cancer and hypersensitive tumors are thought to benefit most from combination therapy. Although endocrine medicines work via distinct mechanisms, they are typically used in combination to improve anticancer efficacy. However, their inconsistent outcomes have been reported [9]. Table 3 represents Randomized phase II/III studies of select anti-estrogen therapies [10].
| Drug | Clinical trial | N | Patient characteristics | Study design | Primary endpoints | Results |
|---|---|---|---|---|---|---|
| Lasofoxifene | Phase II ELAINE I | 103 | MBC ≥ second line including AI/CDK 4/6i with ESR1 mutation | Lasofoxifene vs. fulvestrant | PFS | PFS in the overall population (n=103)
|
| Elacestrant (RAD1901) | Phase III EMERALD | 477 | MBC with 1-2 prior lines of therapy including CDK 4/6i | Elacestrant vs. standard of care (SOC) endocrine monotherapy (fulvestrant/AI) | PFS assessed by blinded independent central review (BICR) in Overall population Subset with ESR1 mutation |
PFS in overall population (n=477)
|
| Giredestrant (GDC-9545) | Phase II acelERA | 303 | MBC with 1-2 prior lines of therapy including at least 1 ET | Giredestrant vs. physician’s choice ET | PFS assessed by the investigator in the overall population | PFS in overall population (n=303)
|
| Giredestrant (GDC-9545) | Phase II coopERA | 221 | Untreated EBC and baseline Ki67 ≥ 5% | Window-of-opportunity phase with 14 days of giredestrant vs. anastrozole followed by 16 weeks of continued ET plus palbociclib | Ki67 change from baseline to week 2 |
Ki67 reduction from baseline to week 2
|
Table 3: Completed randomized phase II/III studies of select anti-estrogen therapies.
Chemotherapy
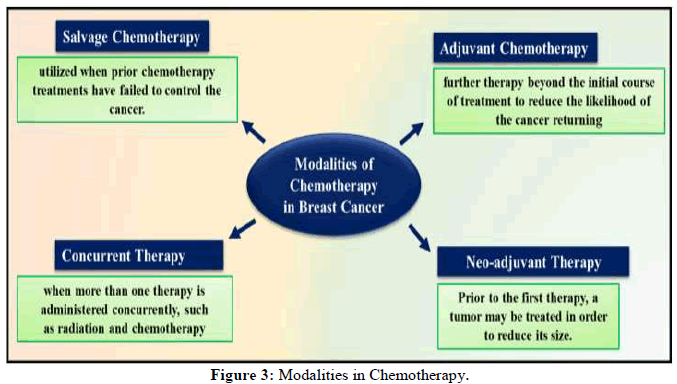
There are many common forms of chemotherapy, which usually include a taxane and an anthracycline. Doxorubicin and cyclophosphamide for four cycles followed by paclitaxel for four cycles, (AC-T) is a typical treatment in the United States. The incidence of breast cancer death has decreased as a result of the extensive use of adjuvant systemic treatments. From single alkylating drugs to polychemotherapy, regimens including anthracyclines and/or taxanes, adjuvant cytotoxic chemotherapy regimens have evolved. Adjuvant chemotherapy is used to destroy any cancer cells that remain after surgery and lower the chance of recurrence. Neoadjuvant chemotherapy is used to shrink the tumor and make it simpler to remove. Chemotherapy is sometimes used in conjunction with other treatments for advanced or metastatic breast cancer to help control the illness and manage symptoms. Adjuvant polychemotherapy or "CMF" regimen, increases survival and significantly lowers the chance of recurrence. Chemotherapy might significantly lower the chance of recurrence in early-stage breast cancer-by around 30%. Adjuvant Chemotherapy (AC), salvage chemotherapy and neo-adjuvant chemotherapy are the cancer treatment methods used in breast cancer patients shown in Figure 3. Salvage chemotherapy is administered after the malignancy has not responded to previous chemotherapy treatments [11].
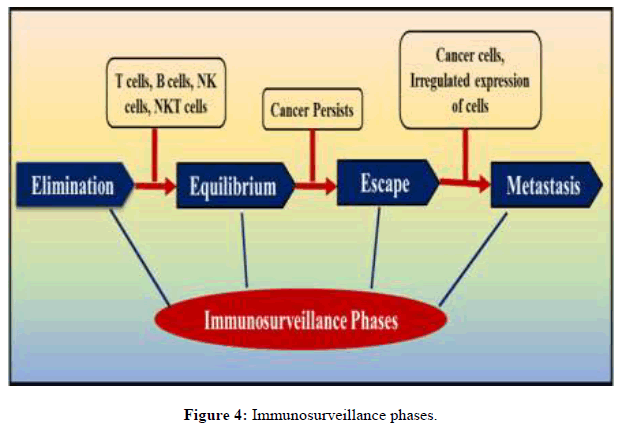
Immunotherapy
Targeted therapy aimed at changing immune system mechanisms to fight a variety of illnesses is called immunotherapy. Immunotherapy is the process of using a patient's immune system to eliminate cancer. The first immunotherapy attempt was launched in the late nineteenth century by two German physicians, Fehleisen and Busch who saw considerable tumour shrinkage after an erysipelas infection. The body's immune system comprises several mechanisms that identify and respond to the presence of cancer cells, a process known as "immunosurveillance". Immunosurveillance comprises three phases: Elimination, equilibrium and escape shown in Figure 4.
Several immunotherapies are now being used for breast cancer treatment. These include: Immune checkpoint inhibitors; cytokine treatments; monoclonal antibodies; breast cancer vaccines; adoptive cellular therapy.
Immune Checkpoint Inhibitors (ICIs): Immune checkpoints are compounds produced by immune system cells that can control the level of immunological activation and play an essential part in controlling autoimmunity. However, tumor cells "skillfully" take advantage of the negative regulatory action of immunological checkpoint molecules in immune cells such as T cells, macrophages, Natural Killer (NK) cells and Dendritic Cells (DCs). The tumor tissue could avoid T-cell-mediated cytotoxic harm via increased expression of checkpoint molecule ligands, causing immune suppression and eventually leading to the incidence, invasion and even metastasis of cancer. Immune Checkpoint Inhibitors (ICIs) are antibodies with monoclonal structures that target particular immune checkpoint proteins on the surface of T cells or tumor cells to stimulate the activation of immune cells and thereby elicit an immunological response against tumor cells.
Some of clinical studies have been complied that are now active or concluded to evaluate the effectiveness of various checkpoint inhibitors. Table 4 summarizes some of these experiments. Various other research studies, either underway or recently finished, examine the efficacy of various other checkpoint inhibitors such as Pembrolizumab, aveluzumab, JS001, Nivolumab plus paclitaxel and bevacizumab, Ipilimumab plus, Nivolumab, Pembrolizumab plus, gemcitabine, Pembrolizumab plus T-DM1 Nivolumab plus radiotherapy [12].
| S. no. | Therapy assessed | Clinical trial phase | Patients | Results |
|---|---|---|---|---|
| 1. | Nivolumab plus paclitaxel and bevacizumab | Phase II | Metastatic BC | Favorable effectiveness and safety. |
| 2. | JS001 | Phase I | TNBC | A good safety record Moderate reaction. |
| 3. | Pembrolizumab plus gemcitabine | Phase II | HER-2 negative advanced cancer | Tumor landscape mapping is recommended for this therapy. |
| 4. | Nivolumab plus radiotherapy | Phase I/II | HER-2 negative metastatic BC | Good safety profile A moderate anti-tumor reaction. |
| 5. | Ipilimumab plus Nivolumab | Phase II | Unresectable or metastatic metaplasia | Response up to three years Variable reactions in patients No new harmful effects were noted. |
| 6. | Pembrolizumab plus T-DM1 | Phase Ib | HER-2 positive metastatic | Positive safety and tolerability profile. |
Table 4: Clinical trials for immune checkpoint inhibitors.
Cytokine therapy: Cytokines are tiny proteins that are released in response to specific stimuli, promoting a variety of cellular functions. Cytokines can have both anti and pro-inflammatory actions, promoting cell growth or death. Cytokines are key regulators of both innate and adaptive immunity, allowing immune cells to interact over short distances. Interleukin-1β, a cytokine present in the tumor microenvironment, can have both anti and pro-tumorigenic actions. Studies on breast cancer models show that IL-1β, shortage leads to tumor regression via recruiting and differentiating inflammatory monocytes. In cancer, IL-1β affects immune cells, angiogenesis, cell proliferation, migration and metastasis. Anti-cancer therapy can stimulate IL-1β production by cancer or immune cells, resulting in opposing consequences on cancer growth.
Interleukin-2 (IL-2) is a cytokine commonly utilized in cancer immunotherapy due to its capacity to stimulate and grow immune cells such as T lymphocytes and Natural Killer (NK) cells. Interleukin-2 is a crucial cytokine that has a wide range of immune-system actions. The most extensively researched cytokine in breast cancer is TGF-β. As a key regulator of numerous processes, such as proliferation, differentiation, migration, immunity and apoptosis TGF-β is a member of the TGF-β superfamily. Strong anti-inflammatory cytokine IL-10 suppresses gene expression, T cell and macrophage cytokine production and antigen presentation. Treatments for breast cancer using cytokines have shown encouraging results. It has been shown that a variety of ILs have potent anti-tumor effects by stimulating immune cells and preventing the growth and spread of tumors [13].
Monoclonal antibodies: The human epidermal growth factor receptor-2 (HER2) is the target of the humanized monoclonal antibody trastuzumab, often known as Herceptin. A member of the receptor family, HER2 stimulates intracellular signal transduction pathways involved in the regulation of cell development through interactions with other receptors and ligands. In 20%-30% of cases of breast cancer, HER2 overexpression has been associated with aggressive tumor characteristics and a dismal prognosis. Trastuzumab is the first oncogene-targeted medicine that has been demonstrated to increase survival in women with HER2-positive metastatic breast cancer. It is also the first humanized monoclonal antibody approved for therapeutic use. Nevertheless, its seeming complexity and poorly known mode of action were noted.
Vaccinations against breast cancer: Cancer vaccines are a different kind of immunotherapy that instruct the immune system to recognize and mount an attack against tumorigenic antigens. Vaccines control or modify the immune system's anticancer responses. Cancer vaccines come in a variety of forms. Some use the immune system or tumor cells from the patient, while others use the patient's cancer antigens to tailor the vaccine specifically to the patient's tumor. Protein-based vaccinations are thought to be the conventional immunization method used to teach T cells to recognize specific antigens that cause tumors.
Several clinical trials are being conducted to evaluate the effectiveness of cancer vaccines in the context of breast cancer. Most of these studies use peptide-based vaccines, while a few look at cell-based vaccines.
Adoptive Cell Therapies (ACTs): Even though cancer immunotherapies are widely accessible, a sizable number of patients eventually experience a decline in their condition and become resistant to these treatments. Therefore, for such patient’s adoptive cellular therapies (ACT, which involves modifying peripheral blood immune cells or intratumoral immune cells might be an option). TIL is thought to indicate an antitumor immune response by the host and is correlated with a favorable clinical outcome in various tumor types, most notably melanoma. TIL Therapy (Tumor-Infiltrating Lymphocyte), TCR-modified lymphocytes and Chimeric Antigen Receptor (CAR) T cells are the three types of Antigen-Presenting Cells (ACTs).
TIL treatment frequently entails the ex vivo expansion of CD8+ or CD4+ T cells, followed by their reemergence in the patient. Genetic modification of a patient's T cells' TCR to recognize tumor antigens specifically is known as "engineered TCR therapy." A patient's T cells can be genetically modified by adding a CAR gene as part of Chimeric Antigen Receptor (CAR) therapy. The latter encodes for a receptor capable of identifying particular cancer antigens. This enables a strong and effective anti-tumor response. First-generation CAR cell testing revealed poor efficacy and unsuccessful immune cell activation. Over this, co-stimulatory signals were included in the design of second and thirdgeneration CAR cells, enabling full T cell activation and expansion [14]. Oncologists could use various predictive program models to help make clinical decisions relating to prognosis. Systemic treatment may be considered after patients are recognized as high-risk but local treatments may be preferred for low-risk patients before systemic treatment.
Gene therapy
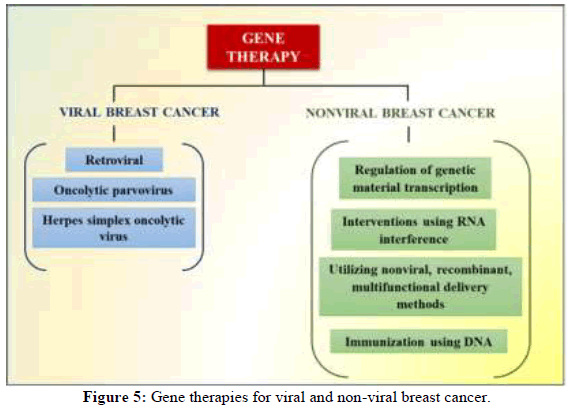
Gene therapy, which is defined as introducing genetic material into target cells via a vector to modify a gene and alter the expression of a gene's product, is another potential strategy for treating cancer. Gene therapy techniques include microRNA, DNA or RNA vaccine, gene editing, transcription factor targeting, microRNA and breast cancer cells, among others. Almost all of these genetic treatments need help getting past the numerous biological barriers that are both intracellular and extracellular. Therefore, a delivery strategy that is usually either viral or nonviral must be taken into consideration for effective nucleic acid transfer as shown in Figure 5.
Gene therapy for viral breast cancer: Viruses make excellent delivery vehicles for gene therapy because they are so adept at transmitting genetic information into cells. Recombinant viruses are developed through genetic engineering to include the desired gene; they are no replicative and need an enclosed cell line to generate particles. Matching viral features to disease targets is becoming increasingly important [15].
Retroviruses and breast tumors: In seropositive individuals, HIV can harm glandular, mesenchymal and intra-mammary lymphoid tissue both directly and indirectly. In vitro studies reveal that HIV replication in human breast cells impedes their development by altering growth hormone, receptors indicating that HIV infection may counteract cancer development in BC cells. Retroviral vectors are typified by their incorporation into the host genome, which induces transgene expression for an extended period. However, insertional mutagenesis and the activation of oncogenes in normal tissues raise some safety concerns. In contrast, if gene expression can be restricted to malignancies, recombinant retrovirus vectors may effectively be used. Direct intratumoral injection can modulate expression, however this method is only practical for tumors that are easily accessible. In addition, the recombinant retrovirus may have a tumor-targeting domain allowing for systemic injection to less accessible metastases.
Parvovirus and breast tumors: A single non-structural protein, NS-1 and two viral capsid proteins, VP1 (83 kDa) and VP2 (58 kDa), are encoded by the small DNA virus known as human parvovirus B19 (B19). Numerous diseases have B19 as their aetiological agent and B19 infection is a major global health concern. B19 infection is more common in hosts with weakened immune systems such as those with AIDS cancer patients undergoing chemotherapy and recipients of immunosuppressive medication for transplant patients. These people cannot typically make neutralizing antibodies to eradicate the virus, which can cause a persistent infection and anemia. Consequently, then it does in the appears that B19 rate of infection in cancer groups is greater than in the normal population.
HSV and breast tumors: The use of viruses that specifically proliferate and kill cancer cells is becoming more and more promising as a therapeutic tool. Oncolytic viruses are developed or manufactured from naturally existing viruses to target and kill cancer cells. Oncolytic viruses not only have preference for cancer cells but they may also be engineered to carry a transgene in addition to their cytotoxic properties. These viruses are then programmed to adopt transcriptional and transduction targeting mechanisms that limit oncolytic vector construct replication to cancer cells while sparing normal cells.
Gene therapy for nonviral breast cancer: Genetic material is usually delivered using one of two ways: Chemically or physically, using a gene gun or injection. A variety of nonviral delivery vehicles, such as polymers, liposomes, peptides or combinations of these, have been developed to protect DNA from degradation and guarantee that it reaches the nucleus. These vehicles are a response to safety and immunogenicity concerns related to viral gene therapy delivery as well as the limitations of physical delivery methods. To match the unparalleled efficacy of viral counterparts, nonviral gene therapy approaches must develop novel ways to enhance the delivery of nucleic acid cargo. A clinical study for breast cancer has evaluated a few physical genes transfer techniques. To compete with viral gene therapy, tactics that offer unparalleled performance nonviral approaches must innovate to enhance their nucleic acid cargo delivery.
The transcriptional regulation of genetic material: The majority of cancer treatments, if not all of them, frequently cause harm to the tissue that surrounds the affected area. Therapeutic effectiveness is frequently constrained by toxicities, even though it is typically essential to ensure the maximum possible delivery of the medication to the tumor. It is generally known that the genetic signature of malignant tissue is distinct from that of adjacent, healthy tissue. Targeting these genetic variations to restrict transgene expression to cells that aberrantly express particular genes is an appealing approach for the gene therapist [16].
Interventions using RNA interference: The transfer of nucleic acid to induce the expression of a therapeutic gene has been the goal of most of the gene therapy techniques discussed above. Interfering with the expression of undesirable genes is another effective genetic treatment tactic. Both siRNA and shRNA have drawn some attention as potential treatments for breast cancer in the experimental setting. They can be used to temporarily or permanently stop a target gene's production [17].
Utilizing nonviral, recombinant, multifunctional delivery methods: The aforementioned delivery options entail intricate chemical and physical procedures to create multipurpose vehicles. Recombinant vector technology has advanced over the past few years. Target cells are transfected with bio-inspired plasmids that carry motifs arranged precisely to produce recombinant biomimetic vehicles that can bind, condense and transport nucleic acid cargo.
Immunization using DNA: Naturally since DNA vaccination does not need long-term gene expression, it circumvents many of the problems associated with conventional nonviral gene therapy. Instead, the goal is to prepare and enhance the patient's immune response so that it can target a specific group of antigens. Conventional pathogenic vaccinations are no longer effective due to safety and adverse effect concerns. Vaccines made from purified subunits, recombinant proteins or synthetic peptides are the main focus of current advances. Even though these vaccines have a very good safety record, even inducing an antibody response can seriously impair their immunogenic effectiveness. The effects of these vaccinations are negligible for many infections particularly intracellular ones. Consequently, there is a "need" to trigger the immune system's cell-mediated response, mostly by cytotoxic T cells or CTLs. DNA vaccination is a highly effective method whereby pDNA encodes a specific antigen for a disease as has been well established. DNA vaccines are usually plasmids that contain unnecessary information, like an antibiotic resistance gene and the replication origin. Furthermore, they are cultured in bacteria that have undergone genetic modification, which adds to the complexity of manufacturing processes and quality control problems [18]. Few studies on gene therapy have been published recently, but many breast cancer strategies are now undergoing clinical trials. Table 5 shows some Molecular alterations 8hat are targetable by FDA/EMA approved drugs [19].
| Gene | Alteration | Drug | Benefits |
|---|---|---|---|
| ERBB2/HER2 | Amplification | Tucatinib + Trastuzumab + Capecitabine | PFS and OS in heavily pretreated HER2-positive metastatic breast cancer patients |
| ERBB2 | Amplification | Capecitabine + Trastuzumab + Tucatinib | Increased of survival in brain metastasis |
| ERBB2 | Amplification | Pyrotinib | Better PFS/ORR than lapatinib with Cap |
| ESR1 | Oncogenic Mutations | AZD9496 or Fulvestrant | Combinations are tested |
| PIK3CA | Oncogenic Mutations | Alpelisib + Fulvestrant | Better PFS than Fulvestrant alone approved by FDA/EMA in mBC with PICK3CA mutation |
| PIK3CA | Oncogenic mutations | GDC-0077 | Evaluating efficacy in PIK3CA mutant hormone receptor-positive HER2-*negative locally advanced and metastatic breast cancer |
| AKT1 | E17K | Capivasertib* | Does finding study pan-AKT inhibitor in breast cancer |
| BRCA1/2 | Oncogenic mutations | Olaparib | In third line and beyond better PFS than TPC |
| BRCA1/2 | Oncogenic mutations | Talazoparib | In third line and beyond better PFS than TPC |
Note: Cap: Capecitabine; mBC: Metastatic Breast Cancer; PFS: Progression-Free-Survival; ORR: Overall Response Rate; OS: Overall Survival; TPC: Treatment of Physician’s Choice, *Not yet approved
Table 5: Molecular alterations that are targetable by FDA/EMA-approved drugs.
We must raise awareness and address the issues causing bias and health disparities as genetic testing become more widely offered and used. In genomic databases and research cohort’s, efforts should be made to be inclusive while honoring individual autonomy and cultural customs and beliefs. To start overcoming medical mistrust, address clinician bias and provide more accessible and culturally competent care and research opportunities, our field must concentrate on recruiting more diverse individuals to provide genetic services tailored to the full spectrum of the patient population [20].
Conclusion
Globally, BC is the primary cause of death for women. It is unlikely that a single therapy will be able to treat every kind of cancer due to BC heterogeneity and the complexity of resistance. In this review, we aimed to summarize and update the current knowledge about breast cancer with an emphasis on its treatment strategies comprises of endocrine therapy, gene therapy for viral and non-viral breast cancer, breast cancer vaccines, monoclonal antibodies, adoptive cell therapies, immune checkpoint inhibitors and T cell receptor therapy. Local and systemic therapies based on surgery are used to treat early stage breast cancer. Surgery is only used in rare circumstances as a palliative measure for metastatic breast cancer patients. Systemic therapies based on chemotherapy are still the main treatment option. On the other hand, traditional treatment options offered very little advantage in terms of survival. The development of immune therapy changed the breast cancer treatment regimen. There is an urgent need to provide the best preventive measures possible, keeping in mind that modifiable risk factors may be essential in reducing the incidence of breast cancer, given the substantial increases in both the morbidity and mortality rates of breast cancer over the past few decades. Breast cancer patient care and clinical results have greatly improved as a result of the ongoing search for prospective biological therapies. Over time, advancements in breast cancer therapy have led to improved patient outcomes and overall survival rates. The kind and stage of the tumor dictate the kind of treatment being employed; certain combination treatments can be preferred. Breast conserving treatment and mastectomy have been proven local treatments for breast cancer in its early stages. Radiation therapy can potentially lower the chance of a recurrence in later stages of breast cancer and avoid mastectomy in cases of early stage breast cancer. Chemotherapy can be administered before surgery to reduce larger tumors assisting the surgeon in doing a more thorough removal of the malignancy. The optimal chemotherapy medicine and prognosis can be determined by assessing how well the cancer reacts to treatment, which is another benefit of chemotherapy. Hormone replacement treatment may shrink or kill cancer cells and if the cancer spreads, can aid in its containment. Following surgery and other therapies, hormone therapy may be employed. Recent clinical trials investigating novel drugs, such as PARP inhibitors, CDK4/6 inhibitors and antibody drug conjugates, show promise in overcoming resistance and targeting specific tumor subtypes. Future research should emphasize optimizing these drug combinations, expanding the scope of clinical trials to include diverse populations and exploring next generation therapies, such as bispecific antibodies and cellular therapies. Nano medicine is one approach that may help overcome some of these limitations with the breast cancer treatment. Nanoparticles are small systems with unique properties that can be used to deliver drugs or as contrast agents. The entire course of treatment is necessary for breast cancer medicines to be effective. A partial course of treatment has a lower chance of success.
Acknowledgment
The authors are thankful to Smt. Kishortai Bhoyar college of pharmacy Kamptee for providing the infrastructural facility to carry out the review work.
Conflict of Interest
There is no conflict of interest among the authors of any sort including financial or non-financial.
References
- Bray F, Laversanne M, Sung H, et al. Ca-Cancer J Clin. 2024; 74(3): p. 229-63.
[Crossref] [Google Scholar] [PubMed]
- Groenendijk FH, Bernards R. Mol Oncol. 2014; 8(6): p. 1067-83.
[Crossref] [Google Scholar] [PubMed]
- Ganesan K, Du B, Chen J. Pharmacol Res. 2022; 178: p. 105974.
[Crossref] [Google Scholar] [PubMed]
- Kerr AJ, Dodwell D, McGale P, et al. Cancer Treat Rev. 2022; 105: p. 102375.
[Crossref] [Google Scholar] [PubMed]
- Sharon S. Gentry Breast Cancer October 2020 Part 4 of 4-Breast Cancer Special Issue Series. August 31 2024.
- Gradishar WJ, Moran MS, Abraham J, et al. J Natl Compr Cancer Netw. 2022; 20(6): p. 691-722.
[Crossref] [Google Scholar] [PubMed]
- Halverson KJ, Perez CA, Kuske RR, et al. Int J Radiat Oncol Biol Phys. 1990; 19(4): p. 851-858.
[Crossref] [Google Scholar] [PubMed]
- Stovall M,, Smith SA Langholz BM, et al. Int J Radiat Oncol Biol Phys. 2008; 72(4): p. 1021-1030.
[Crossref] [Google Scholar] [PubMed]
- Bienia A, Wiecheć-Cudak O, Murzyn AA, et al. Pharmaceutics. 2021; 13(8): p. 1147.
[Crossref] [Google Scholar] [PubMed]
- Patel R, Klein P, Tiersten A, et al. NPJ Breast Cancer. 2023; 9(1): p. 20.
[Crossref] [Google Scholar] [PubMed]
- Akbari ME, Ghelichi-Ghojogh M, Nikeghbalian Z, et al. Ann Med Surg. 2022; 84: p. 104921.
[Crossref] [Google Scholar] [PubMed]
- Rébé C, Ghiringhelli F. Cancers. 2020; 12(7): p. 1791.
[Crossref] [Google Scholar] [PubMed]
- Le I, Dhandayuthapani S, Chacon J, et al. Vaccines. 2022;10(5): p. 816.
[Crossref] [Google Scholar] [PubMed]
- Koşaloğlu-Yalçın Z, Blazeska N, Carter H, et al. Front Immunol. 2021; 12: p. 735609.
[Crossref] [Google Scholar] [PubMed]
- Bretscher C, Marchini A. Viruses. 2019; 11(6): p. 562.
[Crossref] [Google Scholar] [PubMed]
- Nayerossadat N, Maedeh T, Ali PA. Adv Biomed Res. 2012; 1(1): p. 27.
[Crossref] [Google Scholar] [PubMed]
- Tong L, Liu D, Cao Z, et al. Int J Mol Sci. 2023; 24(4): p. 3375.
[Crossref] [Google Scholar] [PubMed]
- Pandya PH, Murray ME, Pollok KE, et al. J Immunol Res. 2016; 2016(1): p. 4273943.
[Crossref] [Google Scholar] [PubMed]
- Vetter M, Kurzeder C. Healthbook TIMES Onco Hematol. 2020; 5(3): p. 26-37.
- Matalon DR, Zepeda-Mendoza CJ, Aarabi M, et al. Gene Med. 2023; 25(6): p. 100812.
[Crossref] [Google Scholar] [PubMed]