Review Article - Der Pharma Chemica ( 2024) Volume 16, Issue 3
Comparison of Regulatory Requirement of Medical Device for Registration in India, USA and Japan
Khyati Patel*, Shruti Jagirdar and Kripa PatelKhyati Patel, Department of Pharmaceutical Regulatory Affairs, Parul Institute of Pharmacy, Vadodara, India, Email: ladani.khyati@gmail.com
Received: 09-Jan-2024, Manuscript No. DPC-24-124775; Editor assigned: 12-Jan-2024, Pre QC No. DPC-24-124775 (PQ); Reviewed: 26-Jan-2024, QC No. DPC-24-124775; Revised: 17-May-2024, Manuscript No. DPC-24-124775 (R); Published: 14-Jun-2024, DOI: 10.4172/0975-413X.16.3.344-348
Abstract
Medical device in recently has been used largely which is concern the safety and effectiveness of the medical device by the regulated country. Medical device standard has been harmonized by the GHTF study group for control of standard of in-vitro medical devices. Even if the same tests have been performed during a process, all medical devices and equipment must go through a mandatory set of tests. The present review discuss about the detail comparative study about the medical device in India, USA and Japan. These regulated authorities make sure that the medical device is safe and efficacious and provide the intended use by manufacturer. Different regulatory guidelines are established for the medical devices by each country for maintaining quality and safety of device. Medical device manufacturing in those countries having large population should be taken seriously and introducing any unsafe product that affect the public health shall be regulated by authorities.
Keywords
Medical device; CDSCO; USFDA; PMDA; GHTF; Registration; Regulation
Introduction
Medical devices nowadays it is acknowledged that medical devices are essential to the medical health department of any developing country that cares about health. They serve a number of functions in the health industry, such as monitoring, treatment/care, restoration and screening and diagnosis. As mentioned in GHTF document SG1 the Global Harmonization Task Force (GHTF) has created a standard definition for medical devices. According the drugs and cosmetics act of 1940, the following definitions are used for "medical devices". All devices similar to instruments, apparatus, appliances, implants, material or articles used alone or in combination, including software or an accessory, intended by its manufacturer to be used especially for human beings or animals which does not provide the primary intended action in human body or animals by any pharmacological or immunological means, however, which could use these methods to support its intended role for one or more of the following particular goals:
• Diagnosis, prevention, monitoring, treatment or alleviation of any disease or disorder.
• Diagnosis, monitoring, treatment, alleviation or assistance for any injury or disability.
• The investigation, replacement or modification or support of the anatomy or of a physiological process.
• Supporting or sustaining life.
• Disinfection of medical devices; and control of conception [1].
Literature Review
The regulatory bodies
Regulatory bodies are the legal frameworks that allow countries to regulate its own regulatory bodies, which are make sure to ensuring the safety, efficacy and quality of medical devices. The national regulatory agencies are listed below and are explained in more detail below(Table 1)[2-4].
| Sr. no | Country names | Regulatory body |
|---|---|---|
| 1 | India | Central Drugs Standard Control Organization (CDSCO) |
| 2 | United State of America | Food and drug administration (Center for device and radiological health) |
| 3 | Japan | Pharmaceutical and Medical Device Agency (PMDA) |
Table 1: Regulatory bodies.
Regulators play an important role in health department; impactful regulatory systems are a vital element of enhancing the system for health and help to provide good public health outcomes," as they "Unstainable regulatory systems themselves can be a barrier to promote safety, effectiveness and quality of medical products."
The regulatory framework's components
The regulatory framework's structure is delineated by the terms "law," "regulation," "standards" and "guidelines," in India, clinical investigation is required for all class B, C and D medical devices if the device is an investigational medical device that does not have a predicate device and is manufactured in the country; or if it is a new IVDMD. However, clinical investigation is not required to grant the import license, if the device is already marketed for at least 2 years in Australia, Canada, Japan, Europe or the United States and the respective CLAs are satisfied with the available clinical evidence. In such cases, CLA may require post-marketing investigation based on subject expert committee’s review and recommendation medical device which are classified in A, B and C are need to be performed clinical investigation in India if the device is a new investigational medical device and is manufactured in India. However, if a medical device has been on the market for more than two years in Australia, Europe, Canada, Japan, United State and Central Licensing Authority are satisfied with already available clinical evidence for medical device then clinical investigation is not required for grant to import license. In such cases, CLA require a post-marketing investigation based on the review and any corrective actions of a subject expert committee [5]. The IMDR talks about all the regulatory aspects of the medical devices, including regulations covering classification, grouping, essential principles and product standards; governing bodies and authorities; registration; manufacture; import; labeling; clinical investigation or clinical performance evaluation; duties of officers and governing bodies; lab registration; sale of medical devices; parameters of classification; fees; notified body; grant of license; quality management system; post-approval changes; PMS and exempt. The Indian Medical Device Rules (IMDR) cover every aspect of medical device regulation, including rules regarding product standards, classification, grouping, principles and regulatory bodies; registration; manufacture; import; labelling; clinical investigation; duties of officers; lab registration; medical device sales; parameters of classification; fees; notified body; license grant; quality management system; PMS, post-approval modifications; and exemptions. The Indian Medical Device Rules (IMDR) cover every aspect of medical device regulation, including rules regarding product standards, classification, grouping, principles and regulatory bodies; registration; manufacture; import; labelling; clinical investigation; duties of officers; lab registration; medical device sales; fees; license grant; quality management system; notified body; PMS, post-approval modifications; and exemptions. The US, one of the largest global markets for medical devices, has very different policies when it comes to granting devices for use in patients. Most low-risk (class I) devices, like stethoscopes, are among the approximately two-thirds of newly marketed devices in the US that are not required to undergo evaluation by the US Food and Drug Administration (FDA). Moderate-risk devices (class II) and some high-risk devices (class III) are cleared by the FDA through the ‘‘510(k)’’ pathway based on their substantial equivalent to previously approved devices without the need for clinical studies. The manufacturer is expected to conduct trials evaluating clinical end points for the highest-risk devices before submitting them for FDA approval through a procedure known as Pre-Market Approval (PMA) [6]. Japan has some of the best healthcare regulatory standards in the world and the country also has the biggest medical device market. Implants, CT scans, MRIs and other imaging software are the most popular devices. The regulatory body in charge of examining medical device applications is the Japan Pharmaceutical and Medical Device Agency (PMDA). Under the Ministry of Health, Labour and Welfare (MHLW), the PMDA is responsible for evaluating the safety of new products, establishing comprehensive regulations and ensuring minority post-market safety. The Pharmaceutical and Medical Device (PMD) Act governs medical device regulations in Japan. This act work on securing safety, quality and efficacy of pharmaceuticals, medical devices, gene therapy and cosmetics. Regulations are very strict in Japan since PMD act imposes strict rules i.e., requirements and standards on the foreign manufacturer and the documents that are published are exclusively in Japanese. An experienced regulatory partner is essential to get your product approved [7].
Country specific definition for medical device
India: All device including an instrument, apparatus, appliance, implant, material or other article, whether used alone or in combination including software or an accessory, intended by their manufacturer to be used specially for human beings or animals, which does not achieve the primary intended action in or on the human body or animals by any pharmacological, immunological or metabolic means, but which may assist in its intended function by such means for Diagnosis, prevention, monitoring treatment, alleviation or assistance for any disease or disorder; investigation, replacement or modification or support of the anatomy or of a physiological process [8].
United State of America (USA): An instrument, apparatus, implement, machine, contrivance, implant, in-vitro reagent or other similar or related article, including a component part or accessory which is; Intended for use in diagnosis of disease or other condition or in cure, mitigation, treatment or prevention of disease, in man or other animals [9].
Japan: Any instrument, apparatus, implement, machine, appliance, implant, reagent for in vitro use, software, material or other similar or related article, intended by the manufacturer to be used, alone or in combination, for human beings, for one or more of specific medical purpose of; diagnosis, prevention, monitoring, treatment or alleviation of disease, also for investigation, replacement or modification or support of the anatomy or of a physiological process and dose not achieve its primary intended action by pharmacological, immunological or metabolic means, in or on the human body, but which may be assisted in its intended function by such means [10].
Classification and regulation of medical device
India: Medical devices besides in vitro diagnostic medical devices, fall into one of the following classes based on the criteria listed in part I of the first schedule: In order to ensure patient safety and health, medical devices need to be able to adhere to strict regulations and specifications. The number of people living in India contributed significantly to the growth rate of medical devices because of the country's healthcare system, rising public awareness of healthcare options and health insurance policies. The Drug Controller General of India (DCGI) and the Central Drugs Standards Control Organization (CDSCO) oversee the regulation of medical devices in the same manner as they oversee drugs. In order to ensure patient safety and health, medical devices need to be able to adhere to strict regulations and specifications (Table 2).
| Class | Risk | Example |
|---|---|---|
| Class A | Low risk | Thermometer |
| Class B | Low to moderate risk | Hypodermic needle |
| Class C | Moderate to high risk | Bone fixation plate |
| Class D | High risk | Heart valve |
Table 2: Classification of medical device in India.
Indian medical devices regulations
According to CDSCO regulation guidelines for medical device; medical devices mentioned in rule 2 must be categorized by the central licensing authority according to the first schedule's specified parameters as well as the device's intended use. A class-by-class list of medical devices will be posted on the Central Drugs Standard Control Organization (CDSCO) website, based on the classification mentioned in sub rule 3: With the caveat that the central licensing authority is free to change the class of any medical device or add or remove items from this list at any time. Important principles for producing medical devices: Medical device manufacturers must adhere to the essential principles of device safety and performance as may be outlined in the guidelines periodically released by the central government's ministry of health and family welfare, taking into account the most recent advancements in science and technology. As long as the guidelines that are to be specified comply with both these rules and the act's provisions.
Medical device product standards
• The medical device must meet the requirements set forth by the Bureau of Indian Standards (BIS), which was founded in accordance with section 3 of the bureau of Indian standards act, 1985 (63 of 1985) or as may occasionally be announced by the central government's ministry of health and family welfare.
• In the event that no applicable standard for a medical device has been established under sub rule 1, the device must adhere to any other pharmacopoeia standards or the standards set forth by the International Electro Technical Commission (IEC) or the International Organization for Standardization (ISO).
• The device must comply with the validated manufacturer's standards if the standards are not specified under sub-rules 1 and 2.
Discussion
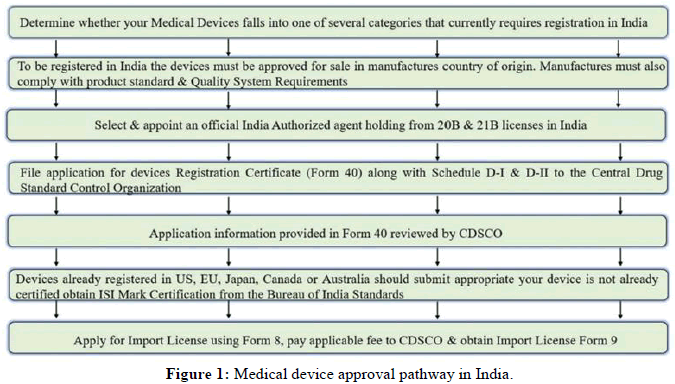
Medical device approval pathways
USA: The FDA staff and the industry are given recommendations by this guidance regarding the content of 510(k) submissions and the process of making decisions regarding the substantial equivalency of devices reviewed under the 510(k) program. The 510(k) decision-making, which has been updated to more closely follow section 513(i) of the FD and C act and pertinent regulations, has been divided into critical decision points that correspond with the organization of the guidance (Figure 1). The following matters are addressed in this document with guidance:
• The appropriate use of multiple predicates.
• The procedures for figuring out whether a newly approved device has a new intended use.
• The process for figuring out whether various technological features raise distinct safety and efficacy concerns.
• The circumstances in which performance data-with a focus on clinical performance data in particular may be required to support a SE determination.
• The development of 510(k) Summaries in order to encourage more transparency in the 510(k) decision-making process (Table 3).
| Class | Risk | Example |
|---|---|---|
| Class A | Low risk of illness | Surgical gauze |
| Class B | Moderate risk illness | Sutures, needle |
| Class C | Significant risk of illness | Peace maker, implantable defibrillators |
Table 3: Classification of medical device in USA.
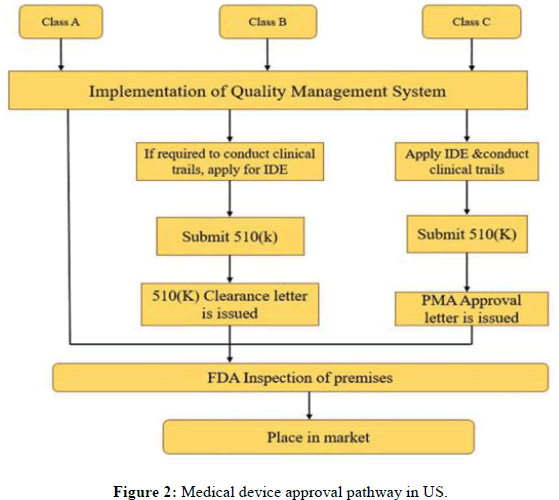
USA medical devices regulations
Pre- Market Approval (PMA) by federal regulations mandate that device manufacturers give the FDA at least 90 days' notice before advertising if they intend to market a scientific machine. There must be clinical evidence. FDA clearance for new Class III devices requires either Level I or Level II proof, as a preferred maximum. It is necessary for researchers to obtain an Investigational Device Exemption (IDE) before using the device in premarket scientific trials. Clinical endpoints can be negotiated with the FDA through talks and design study details can have a big impact on how long it takes and how much it costs to get clinical device approval. PMA evaluation The FDA will determine whether or not the utility is no longer enough to begin a thorough evaluation upon receipt of the PMA. The corporation has 180 days from the date of acceptance for a premarket approval assessment, after which it has 45 days to decide whether to submit the utility and notify the applicant of the submission. A PMA reference variety and the applicant for the reason for the rejection will be the issue if the FDA rejects a PMA as insufficient. The 180-day clock will reset upon resubmission after 45 days of the rejection, during which time applicants can provide additional information. Pre-Marketing Notification (PMN) is granted In order to enable the sponsor to confirm that the device is indeed identical to the one that has been approved and marketed; the PMN is also approved as a 510(k) petition. The confirmation process is rapid. PMN assessment procedure: Sponsor provides CDRH document control center usage fee and two applications (one of which has to be electronic or electronic copy) for PMN. Senders have 180 days to address any questions about digital reproduction and pricing (Figure 2). Upon payment of a fee and obtaining an electronic copy, candidates will be issued a confirmation letter verifying their identity [11].
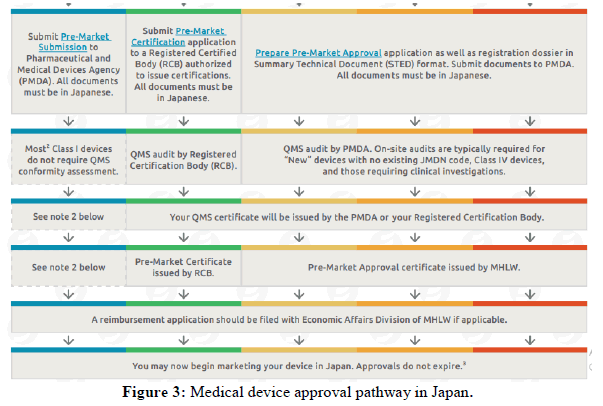
Japan: Medical devices are classified into four classes according to their risk level: Class I (very low risk), class II (low risk), class III (medium risk) and class IV (high danger). To sell medical devices in Japan in accordance with the PMD act, a foreign manufacturer must obtain approval/certification or submit notice through a Japanese Marketing Authorization Holder (MAH) or a Japanese manufacturer appointed by such a foreign manufacturer, depending on the classification (Table 4).
| Class | Risk | Example |
|---|---|---|
| Class A | Extremely low risk | X-ray film |
| Class B | Low risk | MRI, digestive catheters |
| Class C | Moderate risk | Dialyzer |
| Class D | High risk | Pacemaker |
Table 4: Classification of medical device in Japan.
Japan medical devices regulations
In Japan, there are two regulatory authorities that regulate the use of medical devices: The PMDA and the Ministry of Health, Labour and Welfare (MHLW). The MHLW is in charge of regulatory decisions such as product approval guidelines or decisions made in accordance with the PMD act (the act on ensure quality, efficacy and safety of products including pharmaceuticals and medical devices), as well as assessments of whether or not a product qualifies as a medical device. The PMDA, on the other hand, is in charge of post-market safety measures and product reviews. The Japan Medical Device Nomenclature (JMDN) system, which is employed by the PMDA, establishes generic names and codes in compliance with Global Medical Device Nomenclature (GMDN). This system is similar to the product code classification system used by the US food and drug administration. These generic names are then classified into one of four medical device classes based on the potential risk associated with the device, ranging from class I to class IV. The registration procedures differ significantly between device classes. Formerly called Foreign Manufacturer Accreditation (FMA), Foreign Manufacturer Recognition (FMR) is an essential step for any manufacturer planning to market their devices in Japan but producing them abroad. Manufacturers must go through this process, which is different from product registration, in order to sell their medications and medical devices in Japan. A foreign manufacturer registration certificate has a five-year validity period and renewal applications should be submitted about five months prior to the certificate's expiration date, according to the MWHL recommendation. It is the responsibility of the Designated Marketing Authorization Holder (D-MAH) or the Marketing Authorization Holder (MAH) to submit the FMR application (Figure 3) [12].
The comparative study state the difference in market authorization requirement for medical device in India, USA, Japan. One of the most important parameter that determines the market approval process and pathway of medical device and requirement is classification system. Regulations necessary for the approval of new medical devices must protect patient safety while simultaneously offering innovators efficient channels of entry.
Conclusion
Different classification of medical device from low risk to high risk segregation according to predetermined country specific parameters for market authorization. But the comparative study cannot decide that the particular country market approval process is safer medical device in market. By joining the GHTF group for medical device, most country is trying to harmonize their regulation with global requirement.
References
- Manu M, Anand G. Perspec Clin Res. 2022; 13(1): p. 3-11.
[Crossref] [Google Scholar] [PubMed]
- Radhadevi N, Balamuralidhara V, Kumar TM, et al. Asian J Pharm (AJP). 2012; 6(1): p. 55-58.
- George B. Int J Drug Regul Aff. 2019; 7(2): p. 62-66.
- Targhotra M, Aggarwal G, Popli H, et al. Int J Drug Del. 2017; 9(2): p. 18.
- Jefferys DB. Br J Clin Pharmacol. 2001; 52(3): p. 229-235.
[Crossref] [Google Scholar] [PubMed]
- Joshi D, Sharma I, Gupta S, et al. Environ Sci Pollut Res Int. 2021: 10(5): p. 1-22.
[Crossref] [Google Scholar] [PubMed]
- Gupta P, Janodia MD, Jagadish PC, et al. Med Devices: Evid Res. 2010: 25(14): p. 67-79.
[Crossref] [Google Scholar] [PubMed]
- Manikandan K, Kamaraj R. Res J Pharma Technol. 2020; 13(3): p. 1523-1526.
- Moses H, Matheson DH, Cairns-Smith S, et al. Jama. 2015; 313(2): 174-189.
[Crossref] [Google Scholar] [PubMed]
- Tarricone R, Torbica A, Ferre F, et al. Expert Rev Proteomic. 2014; 14(5): p. 707-718.
[Crossref] [Google Scholar] [PubMed]
- Arora M, Baldi A. Indian J Med Microbiol. 2015; 33: p. 2-10.
[Crossref] [Google Scholar] [PubMed]
- Marques MR, Choo Q, Ashtikar M, et al. Adv Drug Deliv Rev. 2019; 151: p. 23-43.
[Crossref] [Google Scholar] [PubMed]