Case Report - Der Pharma Chemica ( 2024) Volume 16, Issue 3
Case Report: Rosuvastatin Induced Rhabdomyolysis and Ticagrelor Causing Acute Kidney Injury in a Tertiary Care Hospital
Shravan R*Shravan R, Department of Chemistry, Andhra University, Visakhapatnam, India, Email: shravanraj98@gmail.com
Received: 02-Jan-2024, Manuscript No. DPC-24-123871; Editor assigned: 05-Jan-2024, Pre QC No. DPC-24-123871 (PQ); Reviewed: 19-Jan-2024, QC No. DPC-24-123871; Revised: 23-Apr-2024, Manuscript No. DPC-24-123871 (R); Published: 27-Jun-2024, DOI: 10.4172/0975-413X.16.3.335-338
Abstract
Drug interactions are a significant cause of adverse drug events as it may cause unexpected side effects or potentiates a significant synergistic reaction. Some drug interactions can even be severely harmful to you hence it stresses the importance to prompt the discontinuation or tailoring of therapeutic regimens to bypass the harmful side effects which could be fatal, here I report two cases of a suspected drug-drug interaction causing an adverse event of Rosuvastatin induced rhabdomyolysis and acute renal failure caused due to the combination with ticagrelor.
Keywords
Drug interactions; Side effects; Rosuvastatin; Acute renal failure
Introduction
Rhabdomyolysis is a well-documented side effect of statin therapy [1,2] rosuvastatin, the newest agent due to its highest potency and efficacy in terms of lipid lowering ability may have a serious side effect in the form of myopathy and the worsening of renal injury. The mechanism of interaction between rosuvastatin and ticagrelor appears to be multifactorial, exact mechanisms underlying SIM is not completely understood but based on the available scientific evidence the following aspects are associated with this condition: Mitochondrial dysfunction, variation in the pharmacokinetics of statins, altered balance in cell degradation and repair, vitamin D deficiency and the primary cause is believed to be the reduced production of coenzyme Q10. It is diagnosed most often as an elevation in creatine kinase of more than tenfold over the upper limit of normal with evidence of renal impairment. Additionally with symptoms that include myopathy, myalgia, myonecrosis and myoglobinuria. In these cases rhabdomyolysis is caused by the damage to skeletal muscles that disrupts muscle integrity and releases muscle components, such as Creatine Kinase (CK), myoglobin, lactate dehydrogenase, aldolase and electrolytes, into the bloodstream. Muscle pain, swelling, weakness and red urine because of increased myoglobin levels. The key laboratory finding is a severely elevated CK levels.
As per the current guidelines of the American College of Cardiology and American Heart Association (ACC/AHA) [3] and the recently executed (PLATO Trial) suggest that in patients with ST-Segment Elevation Myocardial Infarction (STEMI) in severe cases are managed with DAPT involving Ticagrelor on addition with Aspirin as it is more reasonable because Ticagrelor is a directly acting oral antiplatelet drug that acts as a reversibly competitive inhibitor of P2Y12 as its action is more consistent when compared to older antiplatelet drugs along with high-intensity statin therapy for the secondary prevention of cardiovascular events over the long term.
Here ticagrelor being a reversible oral antagonist of the ADP receptor P2Y12. It is rapidly absorbed and metabolized by cytochrome P450 (CYP) 3A4 Therefore, ticagrelor suggests a potential for drug interactions with other CYP3A4 substrates, even though rosuvastatin shows partial affinity to be metabolized by (CYP) 3A4 isoenzyme due to its high potency, ticagrelor has shown to cause acute kidney injury by an unspecified mechanism of interaction which could include genetic differences in the organic anion transporter polypeptides and transportation through p-glycoprotein and increasing the concentration of rosuvastatin which further worsens the renal function and also cause statin induced rhabdomyolysis [4-5].
Case Presentation
Here we present the case of our patient a 58 year old male who came to the emergency department and self-informed with complaints such as tiredness, decreased appetite for the, brown coloured urine output and constipation for the past five days and unable to walk properly due to the weakness in both legs and hip pain for the past 2 days, as per the patient the complaints he mentioned were progressing and worsening day by day (Table 1). On the initial examination by the emergency team the patient was afebrile conscious and oriented with a GCS score 15/15 his vitals on initial examination were as followed:
| Parameters | Score |
|---|---|
| Heart rate | 94 |
| Respiratory rate | 20 |
| SPO2 | 96% |
| Blood pressure | 110/70 |
| GRBS | 232 |
Table 1: Patient diagnostic score report.
Patient past medical history
Patient is a known case of type 2 DM and on treatment had complaints of acute onset of bilateral chest pain, compressive in nature associated with sweating, mild dyspnoea for which he has come to emergency. Patient was clinically evaluated and with the surface ECG and ECHO which were normal in clinical examination with ongoing rest Angina and acute AW-STEMI in rest surface ECG-RWMA with moderate LV dysfunction in ECHO for which ACS, AW-STEMI diagnosis were made and thrombolysis with second generation intra venous thrombolytic agent (Tenecteplase- 30 mg) with loading dose of DAPT and high dose statin.
After 2-3 hours of thrombolysis his surface ECG was not settled and he had ongoing rest angina hence has been shifted to the cardiac catheter lab for high risk emergency CAG+3D-OCT image guided rescue PCI as needed patient was proceeded with right radial artery access high risk emergency CAG on which was showed CAD/critical single vessel disease (Proximal LAD very large ecstatic vessel with 100% thrombotic occlusion with TIMI O flow) with Right dominant system for which high risk plain optimal balloon angioplasty was done(in view of gross vessel mismatched segments with very large long diagonal) and achieved TIMI II-III flow and planned for triple antiplatelet therapy followed by elective image guided optimized complex PCI to LAD after 3-4 days. Since patient had nausea, vomiting, giddiness and he was further evaluated by CTBrain scan which showed normal brain status. Patient was proceeded with right femoral artery access 3D-OCT image guided complex PCI to critical ecstatic proximal LAD was done by using one drug eluting stent (ZES) procedure was uneventful and shifted to the ICCU. Patient was treated with UFH (In catheter lab), LMWH, antiplatelet (Ticagrelor and Aspirin), high dose statin, anti-angina, short and long acting insulin (With periodic sugar monitoring Insulin dose adjustment with the follow up by endocrinologist), beta blocker, ARB, PPI (Figure 1).
Physical examination
• Diabetic keto acidosis
• Myalgia severe
• Myoglobinuria
• Tachypnea
• B/L lower limb calves and thigh muscle tenderness
Clinical investigations and follow up
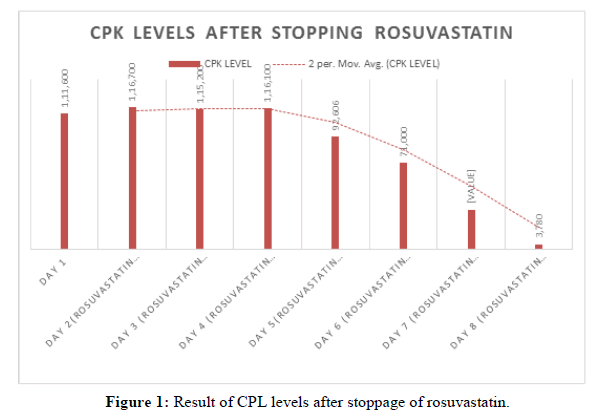
Day 1: CPK-111,600, K+-6.0, ALT-585, Cr-8.4, UCA-ketones +ve (DKA) ABG(MA) Ph-7.3 HC03-10, platelets-98,000.
Day 2: Stopped rosuvastatin, Ticagrelor ongoing. CPK: 116,700 SGOT-1134 SGPT-585 SCr-5.1 Platelets- 51,000 Na+-158, k+ 6.0, cl-116.1, PO-10.7 Urine appearance slightly turbid.
Diagnosis: Acute Kidney Injury and associated electrolyte imbalance, statin induced rhabdomyolysis and rhabdomyolysis associated abnormal LFT
(muscle injury can elevate transaminase levels) (a) and Thrombocytopenia.
DAY 3: Dialysis-2-done Withheld ticagrelor restarted rosuvastatin. CPK: 111,300 SCr-4.1(reduced) SGOT-1275 SGPT-569 Ca+-7.0 urea-122 urine appearance-slightly turbid.
Day 4: Rosuvastatin Stopped Ticagrelor on hold. CPK: 116,100 SGOT-1262 SGPT-667 SCr-3.4(reduced) Na-137 K-4.4 HCO3-155 Ca+-6.5.
Day-5: Rosuvastatin and Ticagrelor on hold. CPK: 92606 (marginally reduced) platelet-37000 HCO3-26.8. Ordered muscle biopsy and HMG COA reductase antibody.
Day 6: Ticagrelor on hold rosuvastatin stopped. CPK: 71000 (Significant drop).
Day 7: CPK: 32,129(Positively significant drop) SGOT-651 SGPT-822 HC03-30.4 Na-118 platelet-68000.
Day 8: CPK-3780 severely reduced after statin stopped.
Day 11: Physiotherapy started.
Day16: HMG COA antibody tested negative (Chemiluminescnce Warfen) confirming self-limited statin induced myopathy.
Day 20: Patient stable, discharged with advised for physiotherapy and renal diet.
Management
Intensive care was given for the patient, treatment with rosuvastatin and ticagrelor was stopped and hemodialysis (SLED) for kidney injury was initiated with right IJV catheter, hypotension was managed with noradrenaline infusion, left vastus lateralis muscle biopsy was done for the patient to rule out autoimmune myopathy, the hypocalcemia caused due to AKI was corrected by administering calcium infusion. Plasmapheresis cycle 1 was done for suspected auto immune myopathy and was ruled out after the urine culture came out positive with enterococcus faecalis and was treated with amoxicillin clauvanate, for anemia two units of PRBC was administered during hemodialysis and the patient was discharged with stopping statin and advised for physiotherapy with a low fat renal safe diet.
Case 2
Patient is a came with the complaints of severe fatigue, nausea and vomiting and decreased appetite for the past one month.
Past medical history
Systemic hypertension: For10 years. CAD: PCI to LAD. Recently developed renal dysfunction after the management with antiplatelet (Ticagrelor and aspirin), high dose statin (Rosuvastatin), beta blockers and ACE inhibitors. And for renal dysfunction patient was treated with diuretics (furosemide and spironolactone), acetylsysteine and sodium bicarbonate over a period of 3 months prior to present admission. This patient is a known case of systemic hypertension for past 10 years, CAD. PCI to LAD Now he is admitted with complaints of severe fatigue with decreased appetite for past one month, nausea, vomiting investigation showed serum creatinine-6.6 mg/dl, urea-191 mg/dl, CPK-40537 Cardiologist opinion was obtained, ECHO showed low normal LV function, mild MR/PAH/TR He was treated with adequate IV fluids considering statin induced rhabdomyolysis, statin was stopped USG Abdomen showed raised renal cortical echoes with well-maintained cortico medullary differentiation, bilateral renal cortical cysts, post cholecystectomy status neurologist opinion was obtained to rule out additional aetiology apart from statin and advised to stop statin and do HMG COA antibody level PET CT showed no definite of metabolically active FDG disease anywhere in whole body Physiotherapy was involved His repeated renal parameters were improving Discharge serum creatinine is 2 mg/dl HMG COA antibodies came out negative and hence proved as self-limiting statin induced rhabdomyolysis [6,7]. He got symptomatically better and was discharged in a stable condition. He was advised to stop the use of statin, continue physiotherapy and follow a low potassium renal safe low fat diet.
Results and Discussion
Two case reports of rhabdomyolysis due to interactions of ticagrelor with statins were found statin-induced myopathy or overall muscle related symptoms during therapy with statins is one of the most frequent adverse events arising from treatment with these drugs. According to various reports A combination of rosuvastatin and ticagrelor is regarded as safe since rosuvastatin is metabolized by CYP2C9 in contrast to ticagrelor, which is a CYP3A4 substrate but rosuvastatin being more potent showed partial affinity to be metabolized by CYP3A4 Ticagrelor being an CYP3A4 inhibitor it could result in an increased serum concentration of rosuvastatin which potentiates side effects and adverse events in some patients. The mechanism behind these events are multifactorial and is believed to be, the cholesterol synthesis blockage which makes the skeletal muscle cell membrane unstable, prenylated protein abnormalities, coenzyme Q10 deficiency causing abnormal mitochondrial respiratory function.
Conclusion
Statins offer several benefits in treating the patients with hypocholesterolemia, even though the risk of developing statin induced rhabdomyolysis and AKI is low, when rosuvastatin and ticagrelor used in combination the incidence is increasing as the presence of triggering factors such as CYP3A4 inhibition, high-dose statins causing increased serum concentration therefore the patients receiving this combination necessitates a monitoring of CPK levels and renal function for a better safety profile.
Disclousre
No conflicts of interest and no financial support or benefits were received only for research/educational purposes.
References
- Danielak D, Karazniewicz lada M, Glowka F. Drugs. 2018; 78: p. 1105-112.
- Gulati M, Levy PD, Mukherjee D, et al. J Am Coll Cardiol. 2021; 78(22): p. 187-285.
[Crossref] [Google Scholar] [PubMed]
- Floyd JS, Brody JA, Tiniakou E, et al. Muscle Nerve. 2016; 54(1): p. 142-144.
[Crossref] [Google Scholar] [PubMed]
- Safitri N, Alaina MF, Pitaloka DA, et al. Drug Health Patient Saf. 2021: 211-219.
[Crossref] [Google Scholar] [PubMed]
- Sakamoto K, Kimura J. J Pharm Sci. 2013; 123(4): p. 289-294.
[Crossref] [Google Scholar] [PubMed]
- Kunakorntham P, Pattanaprateep O, Dejthevaporn C, et al. BMC Med Inform Decis Mak. 2022; 22(1): p. 233.
[Crossref] [Google Scholar] [PubMed]
- Iveta M, Ivana R, Vladimir T, et al. European J Clin Pharmacol. 2022; 78(2): p. 227-236.
[Crossref] [Google Scholar] [PubMed]